Abstract
A care challenge that clinicians and other healthcare professionals face very frequently is the complications of bedridden syndrome. Respiratory involvement readily occurs in these patients for whom medical therapy alone is not sufficient. In this clinical case, the authors describe the results of chest physiotherapy in an elderly patient who had developed complete atelectasis of the left lung, attributable to two mechanisms: obstructive, due to mucus plugging, and compressive, due to pleural effusion.
The patient was accessed in the authors’ Respiratory Rehabilitation Department, San Raffaele Pisana Scientific Institute for Research, Hospitalization and Healthcare (IRCCS), Rome, Italy, with dyspnoea at rest and high O2 requirement (venturi mask fraction of inspired O2: 40%), demonstrated by severe respiratory failure on blood gas analysis (partial pressure of O2/fraction of inspired O2: 155). Physical examination revealed marked reduction of lung sounds, especially on the left side, with diffuse rhonchi.
A chest CT scan was performed to demonstrate complete left lung collapse that would have required invasive therapeutic procedures, such as bronchoscopy. However, given the high risk of periprocedural complications and the patient’s refusal, a chest physiotherapy programme was started. The lung was able to re-expand 7 days later, as evidenced by X-ray and improved gas exchange. The manuscript describes the physiotherapeutic techniques used and collects the main scientific evidence on them. The main purpose is to highlight the role of respiratory physiotherapy as an effective, safe, co-adjuvant treatment, and sometimes alternative to invasive manoeuvres in the treatment of frail patients.
Key Points
1. The article highlights the importance of respiratory physiotherapy, a safe and inexpensive therapy that avoided the use of invasive procedures in an elderly and frail patient with hypoxaemic acute respiratory failure from resorptive atelectasis.
2. Few studies exist on the effectiveness of chest physiotherapy in resolving resorptive lung atelectasis. In this case report, the authors describe the implemented treatment that resulted in the resolution of the mucosal plug. It will be essential to start randomised clinical trials in the future to compare chest physiotherapy with other treatment strategies.
3. Chest physiotherapy should be encouraged from the early stages of hospitalisation in all sufficiently co-operative patients who are elderly, bedridden, or have chronic respiratory diseases, regardless of the reason for admission. It can be considered as a preventive strategy for respiratory complications in the inpatient or as an adjuvant treatment for cases of bronchial hypersecretion.
BACKGROUND
Atelectasis is a kind of lung collapse that might be induced by several factors. Depending on the cause, it can affect only certain areas of the lung (segments or lobes) or the entire lung.1 The main forms of atelectasis are resorptive (or obstructive) and compressive forms.
Resorptive atelectasis results from the presence of airflow obstruction, with the distal residual volume being gradually reduced by shunt phenomena or re-absorption from the blood.2 It occurs in cases of small airway collapse, such as in mucus plugs, neoplasms that narrow the lumen of the bronchi, mediastinal tumours, or compressive lymphadenopathy.1,3
Compressive atelectasis, on the other hand, can also be the result of forces acting externally on the lung parenchyma, causing its collapse. Examples include pleural effusion, pneumothorax, or abdominal distension.
A particular radiological manifestation of atelectasis is the so-called ’rounded atelectasis’. It is visible on the chest CT scan as a roundish area with connecting stripes trying to reach the lung hilum, hence the name ‘comet star sign’.4 It is usually found near a pleural thickening, as in patients with asbestosis or a history of exudative pleurisy.4
This report presents the case of an elderly patient with a double component of atelectasis (obstructive due to mucus plug and compressive due to pleural effusion), who responded excellently to physio-kinetic respiratory treatment without recourse to invasive procedures such as bronchoscopy, usually the gold standard in bronchial unblocking.1
The mucous plug, in this case, represented an important medical emergency because it developed from the left main bronchus and resulted in minimal ventilation of the lung, as shown in chest CT.
Although respiratory physiotherapy has been shown to be effective in the treatment of respiratory disease,5-8 there is limited scientific evidence to support its use in acute and emergency situations.9 In this case, chest physiotherapy represented the resolving treatment of lung collapse and was enabled by the patient’s remaining discrete performance status and by acting as early as possible. In addition, the patient declined more invasive procedures such as bronchoscopy, which would also have been a risky procedure given the concomitant diseases and the severity of respiratory failure.
CASE PRESENTATION
The authors present the case of an 81-year-old female with a history of Parkinson’s disease, atrial fibrillation, and recent bedridden syndrome. Family history was negative for bronchiectasis, cystic fibrosis, or primary ciliary dyskinesia. The patient denied significant pulmonological history, as well as hospitalisations, including in rehabilitation institutions.
The patient was transferred from the Department of General Medicine, San Raffaele Pisana IRCCS, where she had been admitted for dyspnoea, to the Pulmonary Rehabilitation Unit.
Empiric antibiotic therapy was administered in the general medical ward, but within a few days the patient showed progressive deterioration of respiratory failure and underwent CT of the chest, which revealed complete atelectasis of the left lung (Figures 1 and 2).

Figure 1: Chest CT scout image shows opacification of the left hemithorax.
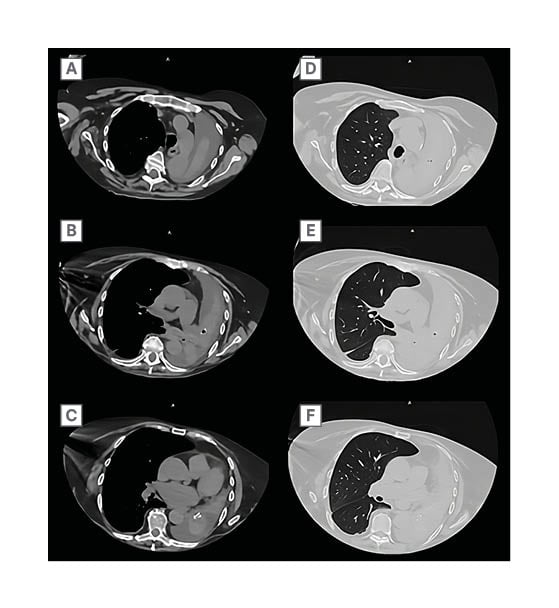
Figure 2: Chest CT mediastinal window (left) and lung window (right).
A and D) Atelectasis parenchyma of the left upper lobe surrounded by fluid. B and E) Hull-level scan highlighting mucous plug in the left main bronchus. C and F) Thickening of bronchial walls and obliteration of left lower lobe branches.
Chest CT showed both an obstructive and a compressive genesis of the lung collapse. The obstructive component was due to mucosal plugs visible in the left main bronchus and extending to the segmental branches of the lower lobe (Figure 2). The compressive component was determined by a pleural effusion that reached the lung apex.
On arrival to the Pneumology Department, San Raffaele Pisana IRCCS, the patient was awake and oriented, with high O2 demand (fraction of inspired O2 of venturi mask: 40%). Blood gas analysis during O2 therapy showed pH: 7.42; pressure of CO2: 45 mmHg; partial pressure of O2: 62 mmHg; bicarbonate: 26.5 mmol/L; and partial pressure of O2/fraction of inspired O2: 155.
Although the patient did not show significant dyspnoea, she desaturated during exercise and in the absence of O2 therapy. Physical examination revealed a marked decrease in lung sounds, especially on the left side, with diffuse rhonchi. Cardiac activity was rhythmic, with a slight amplification of the second tone, but without significant additional murmurs. Dependent oedema was not present. Peripheral pulses were valid and rhythmic. The cough reflex was effective, although attenuated. The peak cough flow measured was 240 L/min, lower than normal but above critical values.
Considering the patient’s age, moderate respiratory failure, concomitant diseases, and therapies (antiplatelet and anticoagulation therapy), invasive bronchoscopy was considered a risky procedure, which was also refused by the patient.
On the other hand, the authors considered the patient’s will and compliance with physical and rehabilitative treatments. After a multidisciplinary meeting (consisting of pulmonary physicians and physiotherapists), a plan of chest physiotherapy was developed and implemented for at least 3 hours per day by the authors’ medical team. At the same time, broad-spectrum antibiotic therapy (meropenem) was administered because of suspected nosocomial infection.
The physiotherapy plan included treatments aimed at the following. Humidification of secretions with a thermal inhaler and a medical aerosol. They were performed daily at least 3 times a day. The duration of the sessions ranged from 5–10 minutes of treatment, depending on tolerance and amount of drug delivered by inhalation (salbutamol 2.5 mg in 0.5 cc; ipratropium bromide 0.25 mg in 1 cc; and beclometasone 400 mcg in 1 mL).
Drainage of the same with active cycle of breathing techniques, consisting of periods of controlled breathing, thoracic expansion exercises, and forced expiration; with l’expiration lente totale glotte ouverte en décubitus latéral (ELTGOL) technique. The manoeuvres were carried out twice a day for a total of 2 hours of treatment, including breaks.
Maintenance and improvement of bronchial clearance by positive expiratory pressures (PEP), frequent postural changes, and diaphragmatic ventilation exercises. The PEP-based treatment that has been used is the PEP-bottle, which has been shown to increase lung volume and removes secretions.10 The device was left with the patient to be used independently under the supervision of the health care team.
The clinical benefit of secretion drainage was immediate, respiratory failure gradually decreased, and a comparative radiograph, taken 7 days later, showed lung re-expansion (Figure 3).
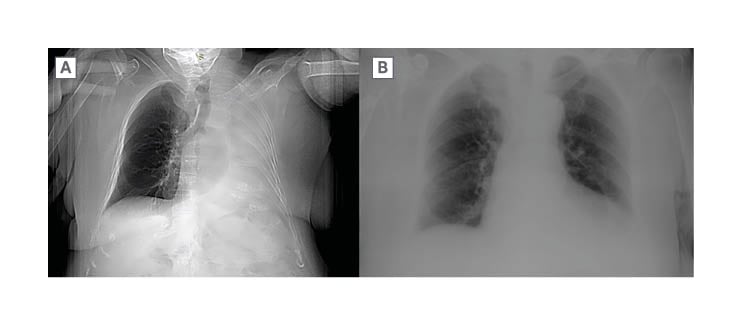
Figure 3: Chest X-ray (A) and comparison after treatment (B).
DISCUSSION
Recurrent pneumonia and recent development of semi-immobilisation were the causes of progressive mucus accumulation. The patient was hospitalised for a long time without mobilisation and physical therapy. This, in combination with a weakened peak cough flow caused by Parkinson’s disease, contributed to the obstruction.
Humidification was necessary before any secretion drainage techniques could be initiated. Humidification techniques have included both the use of a thermal inhaler and a medical aerosol. After this first phase, chest physiotherapy played a central role in the management of this clinical case.
The techniques described have a historical origin, but are still used for patients with respiratory diseases.7 Active cycle of breathing techniques was first proposed in 1979; it consists of 3 phases.11 The phase of controlled breathing is a pause time after the next two manoeuvres, a slow but not prolonged breathing with tidal volume performed through pursed lips. The thoracic expansion exercises step involves a deep, maximal inspiration followed by a 3-second apnoea phase before the slow exhalation. This step is supported by manual chest compressions by the physical therapist or other percussion techniques. By percussion techniques, the authors mean all those manoeuvres aimed at creating a compressive force external to the chest that promotes mobilisation of secretions. These techniques can be manual, exerted directly on the patient by the physiotherapist, or performed through devices (such as those that provide vibrations and oscillations favouring drainage). Examples in the literature are thoracic percussion performed during active cycle of breathing techniques or oscillating devices that generate intra- or extra-thoracic oscillations (orally or external to the chest wall). Internally they create variable resistance within the airway, generating an oscillating positive controlled pressure that mobilises mucus. Extra-thoracic oscillations are generated by forces outside the respiratory system, for example high-frequency oscillation of the chest wall.12
Finally, forced expiration involves open-glottis exhalation by applying a moderate-intensity force after normal inspiration.
It is currently considered the gold standard in physiotherapy for promoting bronchial clearance in patients with chronic respiratory disease.8,13 A study conducted in paediatric patients has shown that a greater amount of sputum is produced in cystic fibrosis compared with conventional physiotherapy techniques.14 However, in this regard, the Cochrane Update 2023 shows no significant differences in outcomes in adult patients with cystic fibrosis between this technique and other physiotherapy treatments.15
A possible application has been hypothesised in patients with hypercapnic respiratory failure undergoing non-invasive ventilation, aimed at increasing the rate of alveolar recruitment by promoting weaning and reducing the length of hospital stay.16
The other technique used was ELTGOL. This technique represents one of the best evidence-based options for secretion removal in patients with bronchiectasis.17,18 It consists of cycles of open glottis exhalations performed in the lateral decubitus, performing breathing efforts starting from normal inhalation reaching the end of exhalation. In the authors’ case, the patient was placed in the left lateral decubitus because secretion drainage is greater in the infralateral lung (i.e., the ‘dependent’ lung), as described in the literature.19
As air passes through the secretions, shear forces are created that promote mobilisation.
In a second phase of therapeutic management of this clinical case, therapies that maintained airway clearance were used, such as exercises based on positive expiratory pressure. Autogenic training and postural drainage were also continued.
The PEP-system, like active cycle of breathing techniques, is based on collateral ventilation. The latter is provided by Kohn’s pores, which allow air to reach a given group of alveoli through adjacent ones, bypassing any obstacles. PEP exercise consists of exhaling against a resistance, creating a force that spans the mucosal plug.
Postural drainage, on the other hand, involves taking a specific decubitus that takes advantage of gravity and bronchial anatomy to move secretions. Although its effectiveness in draining secretions has not been proven, it can be assumed to play a positive role in the ventilation/perfusion ratio of West’s zones by forcing the patient to assume various decubitus positions.20
CONCLUSION
In conclusion, active therapy with the patient and on the patient proved to be a successful strategy in this case, avoiding invasive manoeuvres in an elderly and frail patient. In particular, the authors believe that patients with bedridden conditions can have a great benefit from the early initiation of rehabilitation manoeuvres. Although bronchoscopy remains essential for bronchial unblocking from mucus plugs, chest physiotherapy could be an alternative to consider in selected cases.
Most of the physical therapy techniques that were used in this clinical report are actually implemented in patients with chronic respiratory diseases. Scientific evidence studying chest physiotherapy in cases of lung atelectasis due to secretory obstruction is essentially absent.
This clinical case opens a new therapy scenario, to be further investigated in future randomised clinical trials that may be initiated in intensive care units or pulmonology departments.







