BACKGROUND AND AIMS
The authors present a study that investigated the clinical features and therapy of superior sulcus1-3 non-small cell lung cancer during a 22-year period.
MATERIALS AND METHODS
There was a review of 100 patients who underwent curative surgery for superior sulcus non-small cell lung cancer during a 22-year period (July 1998 to December 2020). Patients with an apical tumour and Pancoast syndrome, superior sulcus tumours with invasion of the chest wall, vertebral body, and/or subclavian arteries met the inclusion criteria. The surgical strategy was determined by the location of the lesion and the architecture of the thoracic inlet. To quantify operative morbidity and mortality, all deaths occurring within 30–90 days following surgery or during hospitalisation were considered. From the date of operation to the date of death or last contact with the patient, overall survival (OS) was calculated. Using the Kaplan–Meier methodology, non-cancer-related fatalities were included in survival curves, and the log-rank test was used to compare survival rates between patient groups. Using Cox proportional hazards regression, the correlation between certain clinical and pathologic features and OS were evaluated.
RESULTS
During the study period, 54 patients were administered induction therapies: 53 patients underwent anterior thoracotomy, 30 underwent Paulson incision, and 8 underwent a combination surgical procedure. There were 84 lobectomies, three pneumonectomies, seven lobectomies with bronchoplastic reconstructions, and seven wedge resections were performed as lung resections. The median number of ribs resected was two (range: 1–5). Chest wall reconstruction was performed on 57 individuals, 23 patients underwent an accompanying vascular resection, and 85 patients underwent radical (R0) resection.
The median length of stay after surgery was 11 days (range: 5–27 days). Overall mortality at 90 days was 6.93%. The average OS lasted 24.3 months (Figure 1). After a median of 3 years of follow-up, the 5-year and 10-year OS rates were 33.9% and 26.4%, respectively. The significantly lower 5-year OS was observed in patients with the nodal disease (46.6% in pN0 versus 13.2% in pN+; p=0.024), without pre-operative treatments (41.0% in patients without pre-operative treatments versus 17.4%; p=0.09), and an anteriorly located tumour (17.4% versus 49.1%; p=0.032). Cox proportional hazards regression revealed superior survival in pT1 (hazard ratio: 4.6; 95% confidence interval: 1.9–11.2; p=0.00076) and R0 (hazard ratio: 4.2; 95% confidence interval: 1.4–12.5; p=0.010) stages.
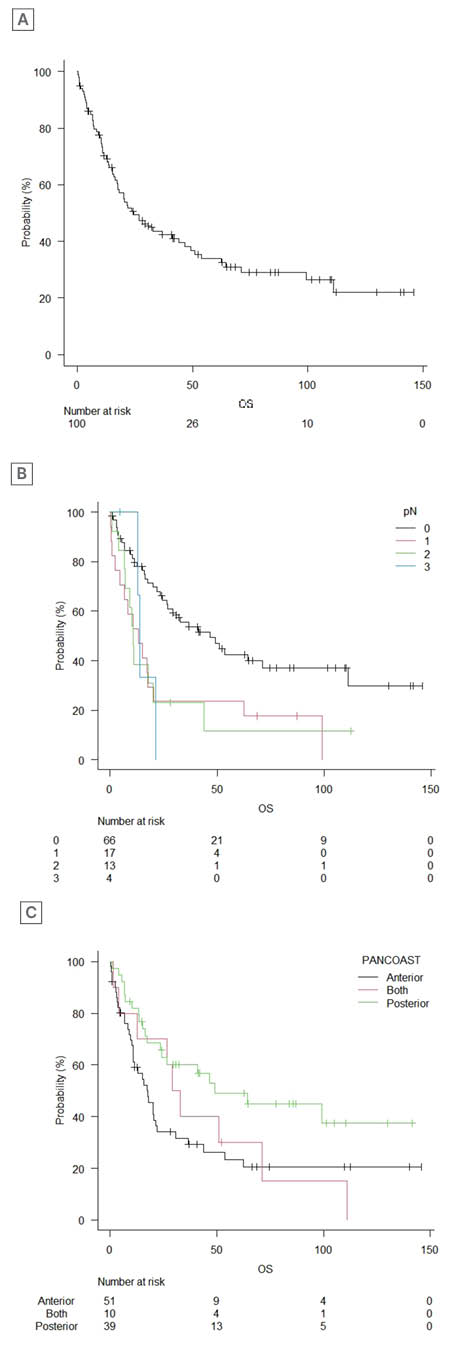
Figure 1: The overall survival of patients.
A) Overall survival. B) Overall survival in patients stratified for nodal disease (log-rank trend test: p=0.00065). C) Location of the tumour (log-rank trend test: p=0.01). OS: overall survival.
CONCLUSION
Superior sulcus tumours continue to be a life-threatening illness that, despite being treatable in a substantial proportion of cases, necessitates complex operations with high surgical risks and a multimodal therapy approach. Physicians should plan the optimal surgical approach to maximise resection completeness and patient survival. Other factors influencing survival are associated with the stage of the tumour, underlining the significance of a comprehensive pre-operative evaluation and candidate selection to identify those who are anticipated to experience a survival benefit.








