One of the most serious complications of silicosis is mycobacteriosis, specifically tuberculosis and, although rare, conditions due to atypical mycobacterium. The incidence of tuberculosis in silicosis cases was 21.8-fold higher than in the general population.1 Among 284 patients with silicosis at the Metallurgical Plant in the Kemerovo region, Russia, silicotuberculosis was present in 19.1% of cases.2 Тhe relationship between the changes in functional parameters and the type of exposure factor is not clear.
AIM
The aim of the study was to evaluate the factors contributing to silicomycobacteriosis (SM) manifestation during 2.5 years of observation.
MATERIALS AND METHODS
Among 250 patients with pneumoconiosis, 32 SM patients (12.8%; 30 with silicotuberculosis, 2 with SM due to atypical mycobacterium) were examined. Of those, 23 were men and 9 were women, the mean age was 61.1±1.7 years, and 36.7% were smokers. Ten of the patients worked as miners and 22 were foundry workers. In difficult diagnostic cases (n=15), the diagnosis was confirmed histologically. SM was the main primary diagnosis (81%). In four cases (13%), SM developed 10–45 years after the diagnosis of silicosis. In 2 patients, silicosis was developed in the presence of inactive tuberculosis. X-ray, computed tomography (CT), complex lung function examination, echocardiography, perfusion scintigraphy, and fibrobronchoscopy were performed. Nine patients received specific therapy (8 during the observation and 1 received a preventive course for >5 years following initial examination). Twelve patients were followed for 2.5±0.8 years (0.5–4.4 years).
RESULTS
SM was diagnosed 1.5±0.5 years after the observed X-ray changes. Fibrobronchoscopy revealed scar-pigmental changes (0.94), infiltration of the bronchial mucosa (0.06), and stenosis of the bronchi (0.33). Obstructive function disorders (0.44; 14/32) were more common than restrictive function disorders (0.19; 2/32; p<0.05). A reduced diffusing capacity of the lungs for carbon monoxide (DLCO) (0.29; 5/17), combined local-diffuse reduction of pulmonary perfusion (0.86; 6/7), pulmonary arterial hypertension (0.54; 16/24), and cor pulmonale (0.46; 11/24) were revealed. Predominant CT signs were: nodule (94%), reticular opacities (56%), and lymphadenopathy with calcifications (41%); rare signs included infiltration (13%) and cavity (6%). A follow-up study revealed stable lung volumes, while DLCO was decreased (Figure 1). Pulmonary arterial hypertension (0.75; 9/12) and cor pulmonale (0.83; 10/12; p<0.05) were detected in patients more often than at the first examination (0.42; 5/12 for both parameters), possibly as a result of the fibrosis progression. Anti-tuberculosis therapy led to positive X-ray dynamics (0.28) and stabilisation (0.42).
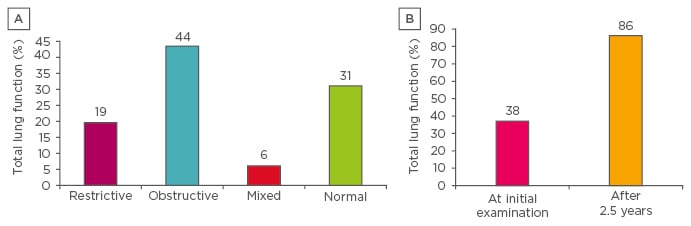
Figure 1: A) Lung function in silicomycobacteriosis patients (n=17). B) The frequency of decrease in the diffusing capacity of the lungs for carbon monoxide during observation of silicomycobacteriosis patients (n=12).
CONCLUSION
SM accounts for 12.8% of patients with pneumoconiosis and was the primary diagnosis in 81% of cases; it was also reported as a complication of silicosis caused by tuberculosis in 13% of cases. Preventive courses of specific treatment improve the prognosis of SM. Annual echocardiography and DLCO monitoring should be carried out to control SM progression.








