BACKGROUND AND AIMS
Perinatal medicine has improved considerably since the 1980s, with the arrival of innovative treatments such as antenatal steroids, exogenous surfactant, and better ventilatory techniques. This has improved survival rates for infants born extremely preterm (EP), particularly among the most immature and vulnerable infants.1Conceivably, these trends might have influenced long-term health outcomes for this group of individuals in opposite directions, with the overall development difficult to predict. Bronchopulmonary dysplasia (BPD), a chronic lung-disease of prematurity, is one of the most common complications of preterm birth,2 leading to varying degrees of compromised lung function in early adulthood.3 The aim of this study was to assess pulmonary outcome at 18 years of age in EP-born and matched term-born control cohorts, born in three different decades and characterised by improvements in neonatal care.
METHODS
Three population-based birth-cohorts of subjects born at gestational age ≤28 weeks or with birth weight ≤1,000 g in 1982–1985 (82–85 cohort), 1991–1992 (91–92 cohort), and 1999–2000 (99–00 cohort) and individually matched term-born control subjects performed spirometry at approximately 18 years of age. Independent sample t-tests were used to compare ‘within-decade’ differences between the EP and term-born groups, whereas one-way ANOVA analyses were performed to compare lung function deficits for the EP-born over three decades.
RESULTS
In total, 118 EP and 111 term-born participants (68% and 80% of eligible subjects, respectively) performed spirometry at approximately 18 years of age. Forced expiratory volume in 1 second (FEV1) Z-scores were lower in EP-born compared to term-born in all three cohorts, deficits being -1.23, -0.68, -0.45 for the 82–85, 91–92, and 99–00 cohorts, respectively (p<0.01; p<0.01; p=0.04). Mean FEV1 Z-scores improved significantly from the 82–85 to the 99–00 EP-born cohort, but not for the corresponding term-born controls (mean differences: 0.67 [p=0.02] and 0.11 [p=1.0], respectively). When splitting the EP-born by BPD, mean FEV1 Z-scores improved significantly from the 82–85 to the 99–00 cohort for subjects with BPD, but not for those without BPD (mean differences: 1.12 [p=0.02] and 0.46 [p=0.59], respectively; Figure 1).
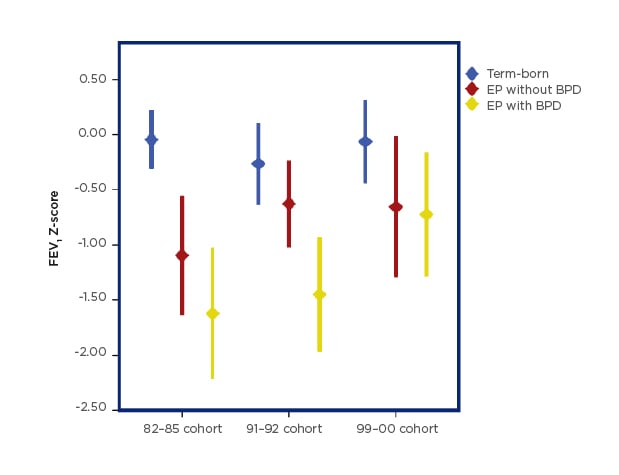
Figure 1: Forced expiratory volume in 1 second (FEV1) Z-score group means with 95% confidence intervals.
BPD: bronchopulmonary dysplasia; EP: extremely preterm.
CONCLUSION
At 18 years of age, survivors of EP birth from all three cohorts had lower lung function than their term-born peers. Pulmonary outcome had improved over the three decades, mainly explained by those with BPD.








