RATIONALE
Chronic obstructive pulmonary disease (COPD) exacerbations are major contributors to the burden of the disease, reducing patients’ quality of life, leading to hospitalisations and increasing mortality.1-3 Prompt treatment accelerates recovery and prevents hospitalisation.4 To achieve prompt treatment, patients need to identify when their symptoms are worsening and seek medical attention. These skills are known as self-management strategies.5,6 When supported by a Written Action Plan and communication with a case manager coaching the patient, self-management strategies can prevent up to 40% of COPD-related hospitalisations.7 However, Written Action Plan adherence rates remain low, with studies reporting adherence <50%.8 Adherence can be improved through more frequent communication, particularly telephone calls from case managers, at the cost of an increased amount of time spent supporting patients.9 Telehealth technologies are a promising strategy to enhance communication with healthcare professionals in severe COPD patients.10 The objectives of our study were to determine whether the use of an interactive phone telesystem increased Written Action Plan adherence to manage exacerbations, which can further reduce hospitalisations in patients from a specialised centre with routine COPD self-management intervention practices.
METHODS
Pilot Study
Forty patients from the COPD clinic at the Montreal Chest Institute, McGill University Health Centre, Montreal, Canada, were enrolled in an initial study. Patients received regular automated phone calls from the telesystem and could contact the telesystem at any time. The telesystem issued alarms to case managers during acute exacerbations. Nurse case managers accessed telesystem call information through a secured online database. Patients kept a symptom diary, recording dates of symptom worsening, treatment use and contact with healthcare professionals. Detailed data from patients’ behaviours during exacerbations were recorded monthly by a third party. Adherence was defined as the patient’s ability to initiate their Action Plan medication by themselves and/or contacting their case manager within 72 hours.
Implementation Scaling-Up Study
The telesystem was then implemented on a large scale to cover >250 patients from a COPD clinic. Healthcare use was assessed with hospital databases.
RESULTS
Thirty-three patients completed the 1-year initial study (12 males/21 females; mean age: 69.0±6.9 years; post-bronchodilator forced expiratory volume in 1 second [FEV1]: 41±13% predicted). A total of 93 symptom-based exacerbations were reported, with the majority of patients reporting ≥2 exacerbations during the year of initial evaluation. Fifty-three percent of patients initiated their Action Plan medication by themselves and 38% contacted their case manager within 72 hours. Overall Action Plan adherence, which includes taking medication as prescribed in the Written Action Plan and/or contacting a healthcare professional within 72 hours, was observed in 72% of exacerbation cases. Exacerbation recovery time was significantly faster for those episodes in which patients adhered to their Written Action Plan (10±6 days for adherent versus 16±10 days for non-adherent patients; p<0.001). Following the large-scale implementation, the use of the telesystem was extended to the caseload of the COPD clinic for a total of 256 patients (117 males/139 females; mean age: 70±9 years; prebronchodilator FEV1: 0.42±0.20% predicted) enrolled in the telesystem. After 1 year of telesystem use, we observed a significant decrease in the number of patients with ≥1 respiratory-related emergency room visits and COPD-related hospitalisations (Table 1).
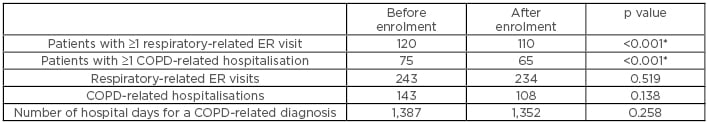
Table 1: Healthcare utilisation before and after telesystem enrolment.
*p<0.05 was considered statistically significant.
COPD: chronic obstructive pulmonary disease; ER: emergency room.
CONCLUSION
Patients already on a self-management programme from a COPD clinic using the COPD telesytem demonstrated higher Action Plan adherence rates than previously reported. The large-scale implementation of the telesystem resulted in a further reduction of COPD-related hospitalisations.








