BACKGROUND AND AIMS
Lung volume reduction is performed in a highly select population of patients with chronic obstructive pulmonary disease (COPD) and severe hyperinflation to improve survival, exercise capacity, and quality of life.1,2 Skeletal muscle loss is a frequent complication in severe COPD that contributes to adverse clinical outcomes, including mortality.3 The authors hypothesized that interventions to ameliorate hyperinflation in severe COPD would improve exercise capacity and restore skeletal muscle mass in these patients.
MATERIALS AND METHODS
Data from the Cleveland Clinic COPD center, Ohio, USA, were analyzed from 2008–2022. Patients were included if they had a CT of the thorax prior to and after bronchoscopic lung volume reduction (BLVR; n=19) or lung volume reduction surgery (LVRS; n=23). An initial CT scan must have been performed within 6 months of the intervention, and a follow-up CT scan must have been performed at least 6 months after the intervention. Pectoralis muscle cross-sectional area (PMcsa), an imaging surrogate for muscle mass, was manually selected using Aquarius iNtuition (TeraRecon, Durham, North Carolina, USA) software based on an attenuation range of -50 to +90 Hounsfield units. Data were compared pre- and post-intervention using paired t-tests with a significant p-value of <0.05. Youden’s optimal cut-off criteria were used to predict an increase in PMcsa post intervention.
RESULTS
Patients with COPD who underwent interventions were 65.3±6.4 (mean±standard deviation) years old, 60.5% male, and 97.7% White. Average forced expiratory volume pre-procedure was 28±7% predicted, total lung capacity was 126±9% predicted, residual volume was 227±40% predicted, and 6-minute walk test (6MWT) was 959.33±307.4 ft. Of the subjects, 57.1% were on supplemental O2, with a mean partial pressure of oxygen in the arterial blood of 67.2±8.2 mmHg. In those patients who underwent BLVR, post-procedure PMcsa was significantly increased by approximately 9% (pre: 23.1+7.1 cm2; post: 25.5+7.3 cm2; paired t-test p=0.03). In those who underwent LVRS, PMcsa was increased by approximately 3%, which was not statistically significant (pre: 26.3+9.2 cm2; post: 27.2+10.1 cm2; paired t-test p=0.58; Figure 1). The average time between intervention and post-CT scan for BLVR and LVRS was not significantly different (BLVR: 0.93+0.53 years versus LVRS: 1.12+0.45 years; p=0.22). Youden’s criteria determined that a 6MWT <1,050 ft was associated with a positive increase in PMcsa post-intervention in all patients (area under the curve: 0.676).
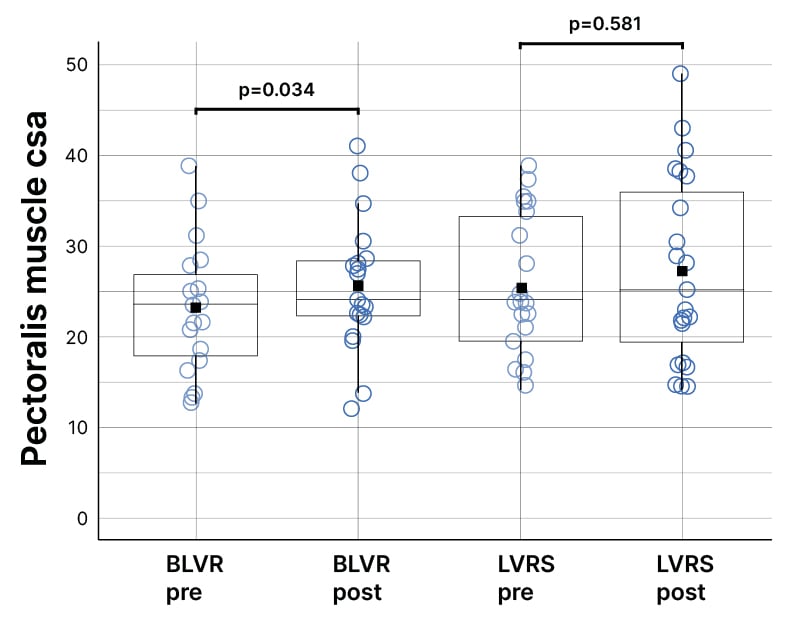
Figure 1: Patients with chronic obstructive pulmonary disease with low 6-minute walk distance at baseline who underwent bronchoscopic lung volume reduction showed improvements in pectoralis muscle cross-sectional area post-procedure.
BLVR: bronchoscopic lung volume reduction; csa: cross-sectional area; LVRS: lung volume reduction surgery.
CONCLUSION
While BLVR and LVRS were both associated with increased pectoralis muscle mass in follow-up CT scans, BLVR was associated with a larger and statistically significant increase. Potential reasons may include the authors’ study’s patients with LVRS being more nutritionally robust than patients with BLVR, or experiencing delayed postoperative response in restoring skeletal muscle mass. The authors’ study also demonstrates that patients with lower exercise capacity, evidenced by a baseline 6MWT of <1,050 ft, may experience significant improvements after lung volume reduction. This echoes the results of the NETT trial, where patients with low exercise capacity had improved outcomes. Further research is needed to identify clinical factors that predict improvements in muscle mass in patients with COPD undergoing lung volume reduction.







