BACKGROUND AND AIMS
Advances in technology in recent years increased the long-term survival rate of patients with chronic respiratory failure. As a result, the number of patients receiving long-term home mechanical ventilation (LTHV) support is increasing worldwide.1 The most important step in the management of patients with home mechanical ventilation (HMV) is to ensure adequate oxygenation and ventilation. Successful care at home requires the presence of trained caregivers and accessibility to medical devices and a care team.2 The aims of this study were, to describe the characteristics of children on LTHV in Istanbul, to compare the patients receiving non-invasive ventilation (NIV) and invasive ventilation, and to evaluate the frequency and risk factors of hospital admission in this population.
MATERIALS AND METHODS
This multicentre, cross-sectional study included LTHV patients followed by paediatric pulmonology divisions of six tertiary hospitals in Istanbul. LTHV was defined as the requirement of a mechanical support for breathing for all or part of the 24-hour day and living for at least 3 months outside the hospital or in a non-acute care setting.3,4 Children on HMV for less than 3 months and children with tracheostomy but without ventilator support were excluded. Demographic characteristics, underlying diseases, presence of concomitant diseases and comorbidities, characteristics of ventilation including location of initiation of LTHV, ventilation parameters, equipment, duration between decision to discharge with LTHV, duration and time period, feeding method, swallowing dysfunction, and nutritional status were recorded. Data regarding emergency department visits and hospitalisations at ward or intensive care unit during the last 12 months were obtained from medical records.
RESULTS
A total of 416 patients were included. The median age was 4.3 years (interquartile range: 2.0–10.3 years). Of the patients, 54.1% were male. While 49.5% (n=206) received NIV, 50.5% (n=210) received invasive ventilation. The median age at initiation of HMV was lower in the invasive ventilation group (10 versus 41 months; p<0.001). The duration between the decision to start and the actual start of HMV was longer in the invasive ventilation group (30 versus 8 days; p<0.001). Most of the subjects in the NIV group (81.1%) received support during sleep while most of invasive ventilation group (55.7%) received continuous life support (p<0.001). In addition to ventilation support, 41.9% of the invasive ventilation group and 28.6% of the NIV group were also on O2 therapy (p=0.002). Neuromuscular diseases (NMD) were the most common primary diagnosis: 35.1% (n=146) of the patients had NMD. Most of children with NMD (n=102) had Type 1 spinal muscular atrophy. HMV decision was made according to polysomnography in 26.9% (n=56) of the children and based on blood, gas, and clinical status in the remaining patients. Data regarding demographic characteristics, underlying disorders, and indications for HMV in NIV and invasive group are presented in Table 1. Fifty-nine percent of the patients were hospitalised (ward or intensive care unit) within the last year. Risk factors for hospitalisation were invasive ventilation, continuous life support, O2 need, tube feeding, and swallowing dysfunction (p=0.002, 0.009, <0.001, <0.001, and <0.001, respectively). Additionally, 65.2% of the subjects (n=86) with no hospitalisation in the last year had no swallowing dysfunction, whereas 59.1% (n=143) of subjects who had hospitalisation had swallowing dysfunction (p<0.001).
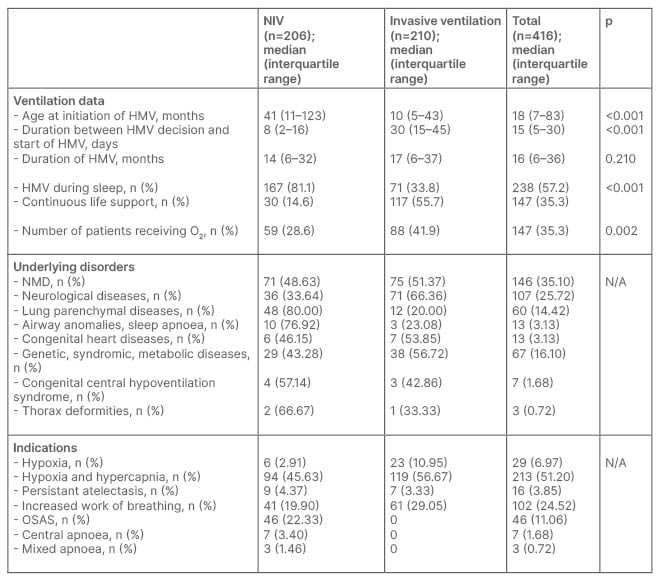
Table 1: Demographic characteristics, underlying disorders, and indications for home mechanical ventilation in non-invasive ventilation and invasive group.
HMV: home mechanical ventilation; NIV: non-invasive ventilation; NMD: neuromuscular diseases; OSAS: obstructive sleep apnoea syndrome.
CONCLUSION
Multidisciplinary follow-up of children on LTHV with complex medical problems is important in order to decrease morbidity and mortality.








