BACKGROUND
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death worldwide and is predicted to be the third leading cause of death by 2020.1 Most COPD patients have at least one comorbid condition that further complicates the evolution and management of the disease. COPD is currently regarded as a systemic condition and is linked to several comorbidities with major clinical importance, including cardiovascular, metabolic, and gastrointestinal complications.2 At least one comorbidity of clinical relevance is found in 78.6% of COPD patients, two in 68.8% of patients, and ≥3 in 47.9% of patients, with cardiovascular comorbidities being the most predominant.3 This underlines the need for multidimensional assessment and complex management of COPD patients.4 The aim of the study was to evaluate and analyse the prevalence and clinical significance of COPD comorbidities in Moldova.
METHODS
The study was conducted in 435 patients with COPD. Spirometric data were analysed, including forced expiratory volume in 1 second, forced vital capacity, and a ratio of both, and were assessed by multidimensional indexes, including BODE, ADO, BODEx, CODEX, and DOSE.
RESULTS
The results showed that 38.62% of patients had heart failure, 50.11% had hypertension, 23.45% had coronary artery disease, 10.11% had diabetes, 1.15% had renal failure, 3.22% had rheumatoid arthritis, 4.83% had depression, 4.37% had cognitive impairment, 29.89% were obese, and 3.22% had cachexia. Only 24.65% of patients did not have any comorbidities. Patients with one comorbidity represented 23.73% of the study sample, two comorbidities were present in 24.19%, and ≥3 comorbidities were present in 27.42%. The Charlson Comorbidity Index (CCI) had a medium negative correlation with 6-minute walking distance (r=-0.37; p<0.001) and a weak correlation with the rate of exacerbations (r=0.17; p=0.016). CCI had a strong correlation with ADO (r=0.75; p<0.001), a moderate correlation with BODE (r=0.30; p<0.001), and a weak correlation with BODEx, CODEX, and DOSE (Figure 1). CCI also had a medium correlation with St. George’s Respiratory Questionnaire activity (r=0.36; p<0.001), impact (r=0.34; p<0.001) and total (r=0.37; p<0.001) scores, and the overall quality of life assessed by St. George’s Respiratory Questionnaire and CCQ.
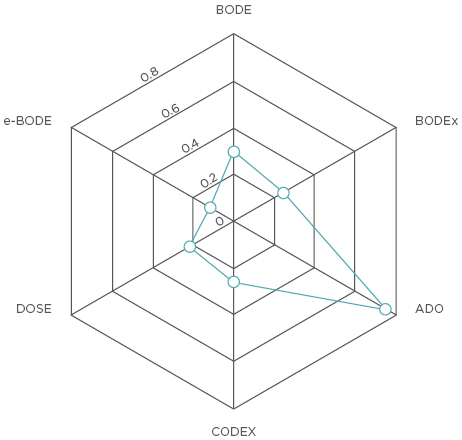
Figure 1: Correlation between multidimensional indexes and the Charlson Comorbidity Index in the study population.
CONCLUSION
COPD patients often have one or two comorbidities of clinical significance that are predominantly cardiovascular and metabolic in nature. These two groups of disease commonly coexist together and potentially share underlying pathophysiological pathways. COPD patients with comorbidities tend to have a poorer health-related quality of life and, as shown by this study, such comorbidities can be assessed by multidimensional indexes, such as ADO, BODE, and others.








