Abstract
Maternal ovarian torsion in pregnancy is very rare. Non-specific symptoms, signs, and imaging findings make the diagnosis difficult. A delay in diagnosis can lead to irreversible damage to adnexa and fetal compromise. Difficulties encountered in the diagnosis and management of adnexal torsion in the third trimester of pregnancy are highlighted in this article.
INTRODUCTION
Adnexal torsion usually occurs in ovaries with functional cysts or tumours. Torsion of normal adnexa is rare during pregnancy, especially in the third trimester. The diagnosis of adnexal torsion is difficult to establish during pregnancy from symptoms, signs, and imaging techniques.1 The patient usually presents with non-specific symptoms like abdominal pain, nausea, and vomiting, which can be easily mistaken for appendicitis, cholecystitis, pyelonephritis, or preterm labour. This can lead to delays in diagnosis and surgical management, resulting in loss of adnexa as well as fetal compromise.2
We report the case of a primigravida at 31 weeks’ gestation, admitted to a tertiary care hospital with a presumptive diagnosis of acute appendicitis, which turned out to be torsion of a normal adnexa.
CASE PRESENTATION
A 26-year-old primigravida at 31 weeks’ gestation was admitted with a history of right lower abdominal pain, nausea, and vomiting of 1-day duration. She was seen in a secondary care hospital earlier in the day with a presumptive diagnosis of appendicitis. After receiving analgesics, she felt better, refused surgery, and went home against medical advice. After 6 hours, the pain got worse, and she became febrile and presented to our hospital. She was assessed by the obstetrician and the surgeon in the emergency room. The pain was severe, mainly in the right lumbar and lower abdomen with nausea, vomiting, and fever. There were no urinary symptoms or vaginal discharge, bleeding, or leaking. She felt normal fetal movements.
On examination, the patient was febrile and in distress. Her blood pressure was 120/80 mmHg, pulse 116/min, temperature 38°C, and oxygen saturation was 100% in room air. Abdominal examination revealed a relaxed gravid uterus corresponding to 30 weeks with tenderness, rigidity, and guarding in the right lower abdomen. A cardiotocogram showed reassuring fetal heart tracing with no uterine contractions. An abdominal ultrasound scan revealed fetal parameters corresponding to the gestation with normal amniotic fluid and fetal movements. The appendix was not visualised and no adnexal mass was detected.
The patient’s haemoglobin was 10.2 g/dL with a white cell count of 9,500/mm3. C-reactive protein was 2 mg/L. Blood group was B Rh+. Urine analysis was normal. With a provisional diagnosis of acute appendicitis, the general surgeons took her for laparoscopy. Intraoperatively, the appendix was found to be normal in appearance with a twisted right ovary and tube (Figure 1) and the gynaecology team was called in.
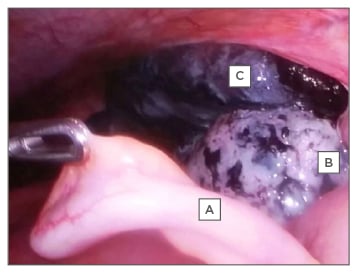
Figure 1: A) Normal appendix; B) necrotic ovary; C) necrotic fallopian tube.
As access to the adnexa was limited, and manipulation was technically difficult and risky due to the enlarged uterus, we proceeded with a subumbilical midline laparotomy. There was minimal haemoperitoneum; a sample was taken for cytology and culture. Both ovaries were found to be normal in size, the right ovary and tube were twisted three times, and the ovary and tube looked gangrenous and non-viable. As there was no evidence of functioning vascular supply on untwisting the ovary, a right salpingo-oophorectomy was performed. Intraoperative antibiotic (injection cefuroxime 1.5 mg at intubation) was given followed by oral cefuroxime 500 mg twice-daily for 5 days. As a prophylaxis against preterm labour, she was given an indomethacin suppository 100 mg preoperative, followed by an injection of hydroxyprogesterone hexanoate (Proluton Depot, 250 mg/mL x 1 mL) once-weekly for 4 weeks.
The patient had an uneventful stay in the hospital and was discharged on postoperative Day 4. Peritoneal fluid cytology was normal. High vaginal swab, urine, peritoneal fluid, and blood cultures were negative. Histopathology confirmed a gangrenous fallopian tube and ovary (Figure 2).
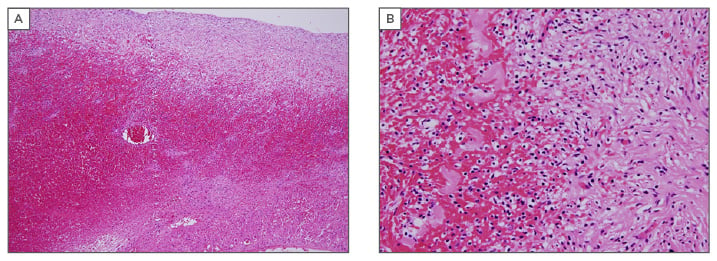
Figure 2: A) Haemorrhage and necrosis of ovary H&E x 20; B) haemorrhage and necrosis of ovary.
H&E x 40.
H&E: haemotoxylin and eosin.
The pregnancy continued without problems until 38 weeks when she developed pre-eclampsia and underwent induction of labour with prostaglandin E2 gel. She delivered vaginally a baby girl weighing 2,480 g (<10th centile) with Apgar scores 9 and 10 at 1 and 5 minutes, respectively. Delivery was complicated with primary postpartum haemorrhage (blood loss 1.5 L) due to uterine atony, which was managed successfully with oxytocics.
DISCUSSION
Torsion of adnexa in pregnancy is a rare cause of gynaecological emergencies where the adnexa rotates on its pedicle and compromises its blood supply, leading to stasis, venous congestion, haemorrhage, and necrosis.3 The reported incidence is 1/1,000 during pregnancies, occurring mostly during the first trimester, especially in women undergoing ovulation induction for infertility and in those diagnosed early to have an ovarian cyst.4 Accurate diagnosis and early surgical intervention is essential as it facilitates conservative surgery, saving the adnexa, especially in young women where preservation of future fertility is of utmost importance.5
Diagnosis of ovarian torsion in advanced pregnancy is challenging as the symptoms, signs, and imaging findings are non-specific and can be confused with other acute abdominal conditions. Clinical examination is usually hampered by the anatomical displacement of the abdominal organs by the enlarged uterus. Ultrasound imaging of the ovaries is technically more difficult during pregnancy, especially in advanced gestation.1,6 This leads to delay in surgical intervention, resulting in increased maternal and fetal morbidity. A combination of magnetic resonance imaging findings and lack of perfusion of ovarian parenchyma on colour Doppler sonography appears to be promising in the diagnosis of ovarian torsion in pregnancy.1,7 However, the absence of Doppler signals may be a late sign and the presence of signals within the ovary does not exclude ovarian torsion.8,9
The type of surgical approach during pregnancy remains controversial and it depends on the availability of resources, the skill of the operator, and the patient’s suitability. Several reports show that laparoscopy is technically feasible and as safe as laparotomy, even in the third trimester, with the additional advantages of minimally invasive surgery.10-12 Simple detorsion is sufficient even in dark purple or black coloured ovary if vascular supply returns on untwisting the pedicle. Salpingo-oophorectomy may be necessary depending upon the degree of ischaemia and necrosis.7 In our case, we proceeded with laparotomy and salpingo-oophorectomy, as laparoscopy was technically difficult and the tube and ovary looked gangrenous and non-viable even after detorting.
CONCLUSION
Adnexal torsion may occur even in the absence of ovarian cysts. Torsion of normal adnexa should be considered as a differential diagnosis of acute abdominal pain in the third trimester of pregnancy, although rare. Prompt diagnosis and early surgical intervention might help in the conservation of adnexa, preservation of fertility, and reduction of maternal and fetal morbidity.








