Abstract
The present study reports a complete hydatidiform mole presenting with ovarian hyperstimulation syndrome after dilatation and evacuation. A 30-year-old female came to the emergency room with abdominal pain and genital bleeding at 14 weeks of pregnancy. Ultrasonography revealed vesicular cystic swelling of chorionic villi with high human chorionic gonadotrophin (625,000 IU/L). Dilatation and evacuation was performed. Symptoms of ovarian hyperstimulation syndrome appeared on the 8ᵗʰ day after dilatation and evacuation, and bilateral enlarged multicystic ovaries were found, measuring 13.07×8.45×9.77 cm on the left and 9.02×8.45×5.5 cm on the right. The cysts gradually reduced in size and finally disappeared at Day 42, and human chorionic gonadotrophin reached below cut-off value at Day 72.
Key Points
1. Although ovarian hyperstimulation syndrome (OHSS) accompanied by natural pregnancy is rare, in case of hydatidiform mole there is cystic proliferation of chorionic villi and release of excess human chorionic gonadotrophins, by which ovaries are hyperstimulated.
2. This manuscript describes clinical assessment, specific laboratory parameters, treatment options, and positive consequence in OHSS after dilatation and evacuation of hydatidiform mole.
3. Spontaneous onset of OHSS can be a complication of hydatidiform mole and the condition worsens after dilatation and evacuation. Clinicians should be aware of ovarian cysts accompanied OHSS, as clinical assessment and timely intervention is helpful to avoid complications.
INTRODUCTION
Ovarian hyperstimulation syndrome (OHSS) is common following ovarian stimulation by clomifene citrate or follicle stimulating hormone.1 This stimulation causes exposure of ovaries to human chorionic gonadotrophins (hCG) or leutinising hormone. As ovaries are hyperstimulated, there is increased production of pro-inflammatory mediators like vascular endothelial growth factors (VEGF). Due to increased endothelial permeability by VEGF, clinical manifestations occur, such as ascites, pleural effusion, haemoconcentrations (increased haematocrit >45%), and in severe cases thromboembolism.2 OHSS is rare in naturally conceived pregnancy, but any type of molar pregnancy, complete or partial mole, can be complicated by OHSS. Usually this condition worsens after dilation and evacuation (D&E).3
CASE REPORT
A 30-year-old female, mother of 2 children (last child aged 5 years), with naturally conceived pregnancy, presented to the emergency room at 14 weeks of gestation with complaints of abdominal pain and genital bleeding for 6 hours. On admission, patient was mildly anaemic, with pulse rate of 90 beats/min, blood pressure of 110/65 mmHg, height of 154 cm, weight of 42 kg, and BMI of 17.71 kg/m2. Uterine height was at the level of the umbilicus, which is larger than the corresponding gestational period of 14 weeks. Genital bleeding was present and ultrasonography revealed ‘snow storm’ appearance, suggestive of cystic swelling of chorionic villi, and absence of foetal parts. Laboratory parameters revealed white blood cells of 10,600 /µL, haematocrit of 40%, albumin of 4.3 mg/dL, and hCG of 625,000 IU/L (normal <5 IU/L). Considering all these parameters, including clinical features at 14 weeks gestation of abdominal pain and genital bleeding with increased fundal height; radiological findings of ‘snow storm’ appearance suggestive of cystic swelling of chorionic villi, and absence of foetal parts; and hCG laboratory value of 625,000 IU/L, the authors diagnosed this as a case of hydatidiform mole. D&E was subsequently performed.
After evacuation, the authors found a profuse amount of uterine contents, which were cystic without any foetal component. Histopathology revealed complete hydatidiform mole. After evacuation, hCG decreased to 22,803 IU/L and 12,803 IU/L at Day 2 and Day 4, respectively. It gradually reached cut-off level of less than 5 IU/L at Day 72 (here cut-off level is a value of hCG, where below this level is considered negative or not detected and above this value is positive, with a normal value <5 IU/L).
On the 8ᵗʰ postoperative day, the patient came for an outpatient consultation with complaints of bloating, mild abdominal pain, and palpable lump. They had no complaints of nausea, vomiting, or shortness of breath. Ultrasonography revealed bilateral enlarged multicystic ovaries, measuring 13.07×8.45×9.77 cm on the left and 9.02×8.45×5.5 cm on the right, with a small amount of pelvic collection (Figure 1). Serum oestradiol level was 2,582 pg/mL and other laboratory parameters, including haematocrit, serum albumin, liver enzymes, and serum creatinine were normal. The authors diagnosed bilateral multilocular cysts with OHSS. As it was of moderate variety, it was treated on an outpatient basis. The patient was counselled properly regarding treatment and consequences of severe signs/symptoms. Proper intake of fluids and analgesics for pain relief were ensured. The patient came for regular visits with baseline investigations.
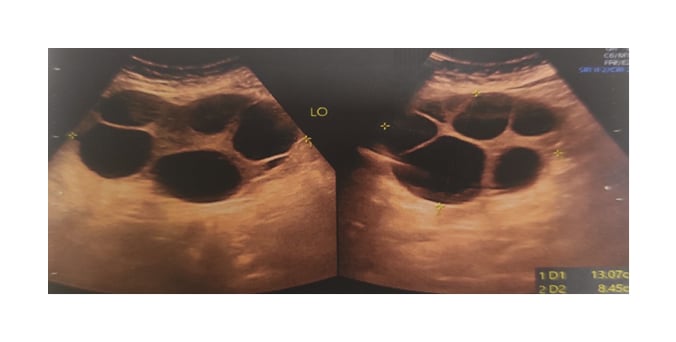
Figure 1: Left-sided multicystic ovary measuring 13.07×8.45×9.77 cm.
With all these measurements, the patient recovered completely. The cysts gradually reduced in size and finally disappeared on Day 42, and hCG reached below cut-off value on Day 72 after D&E.
DISCUSSION
The incidence of OHSS varies for different protocols of infertility treatment. The greater the involvement of stimulation, the higher the incidence becomes. In conventional in vitro fertilisation (IVF), approximately one-third of cases may be affected. Moderate to severe OHSS varies from 3.1–8.0%.4 The 14ᵗʰ European IVF Monitoring Report revealed incidence of hospitalisation due to OHSS is 0.3%.5 Although OHSS accompanied by natural pregnancy is rare, it can be observed in case of hydatidiform mole where there is cystic proliferation of chorionic villi and release of excess hCG, by which ovaries are hyperstimulated. Hydatidiform mole may be either partial or complete, and most cases worsen after D&E. In the authors’ study, OHSS was secondary to complete molar pregnancy with markedly elevated oestradiol level.
In case of OHSS, there is increased production of pro-inflammatory mediators such asVEGF.2,3 Increased vascular permeability leads to accumulation of fluid in the third space, manifested by dehydration, hypovolaemia, oliguria, haemoconcentration, reduced osmolality, electrolyte imbalance (including hyponatraemia and hyperkalaemia), ascites, and pleural or pericardial effusion. In severe cases, there is a loss of 20% of calculated volume.6 In the authors’ study, they diagnosed the case as moderate OHSS. There was no ascites or pleural effusion due to low BMI (17.71 kg/m2), and intrabdominal pressure was high as larger cysts occupied the abdominal cavity and suppressed leakage of fluids.
Sizes of ovarian cysts are variable. Suzuki et al.7 reported the largest size of a 30 cm cyst, which normalised within 1 month. In this study, the authors found bilateral enlarged multicystic ovaries measuring 13.07×8.45×9.77 cm on the left and 9.02×8.45×5.5 cm on the right, which returned to normal size on Day 42 after D&E. The duration of reduction of size is not always related to size, as a larger cyst may become normal in a short time, but a smaller cyst may need more time.
Treatment is mostly conservative, as in mild to moderate cases, outpatient management is appropriate. Proper counselling is needed regarding consequences of disease, signs of severity, maintenance of proper hydration, analgesics for pain relief, and regular follow-up with baseline investigations.
Clinicians should be aware of signs and symptoms of severity, which should be explained properly so that the patient can seek medical treatment earlier.
Signs of severity are increasing abdominal distension, shortness of breath, hypotension, tachycardia, reduced urinary output (<1,000 mL/24hrs), weight gain and increased abdominal girth, and increasing haematocrit (>45%). Females with severe OHSS are at risk of thromboembolism, and thromboprophylaxis should be prescribed. Prophylactic anticoagulation by warfarin or low molecular weight of heparin is indicated. Paracentesis may be needed for tense ascites. In the authors’ study the patient was treated conservatively with appropriate counselling and care, and recovered completely.
CONCLUSION
Spontaneous onset of OHSS can be a possible complications of hydatidiform mole. The condition worsens after D&E. The clinicians should be aware of ovarian cysts accompanied OHSS. Clinical assessment and timely intervention is helpful to avoid complications. Most of the cases resolve spontaneously and sizes of ovaries become normal even when they are larger.







