Abstract
Background: Approximately 15% of all pregnancies (about 20 million) suffer from acute severe obstetric complications. The first 24 hours postpartum represent the period with the highest chance of mortality. The most evident complication is haemorrhage, solely accounting for 27% of all maternal deaths worldwide. Haemorrhage occurring postpartum accounts for 73% of all cases. Primary postpartum haemorrhage (PPH) is defined as the loss of at least 500 mL of blood after vaginal delivery or 1,000 mL of blood after Caesarean section within 24 hours of delivery.
Aim: This cross-sectional study aims to evaluate the incidence and determine risk factors of PPH after vaginal delivery in Kasr Al Ainy University Hospital, Cairo, Egypt.
Methodology: The study is a multivariate cross-sectional study. Single population proportion formula was used to determine the sample size in accordance with inclusion and exclusion criteria. Data was collected via assisted questionnaires, and results were statistically interpreted with a confidence interval of 95% to gather the odds ratio (OR) of significant risk factors of PPH. The SPSS® (IBM, Armonk, New York, USA) statistical package was used.
Results: PPH incidence in Kasr Al Ainy in the period of this study was 8.1%. Atonic factors were implicated in 67% of all PPH after vaginal delivery. Most evident risk factors were prolonged labour (OR: 5.1), history of previous PPH (OR: 4.25), hypertension (OR: 2.53), and age ≥35 years (OR: 2.29), respectively.
Conclusion: The authors’ research concluded that most cases of PPH were mainly of atonic causes, with prolonged labour being the most evident risk factor.
Key Points
1. Approximately 15% of all pregnancies (about 20 million) suffer from acute severe obstetric complications.
2. The most evident complication is haemorrhage, solely accounting for 27% of all maternal deaths worldwide, with postpartum haemorrhaging accounting for 73% of all cases.
3. This cross-sectional study aims to evaluate the incidence and determine risk factors of primary postpartum haemorrhage after vaginal delivery in Kasr Al Ainy University Hospital, Cairo, Egypt.
BACKGROUND
Every year, over 300,000 females die due to complications in pregnancy and childbirth, and approximately 15% of all females who are pregnant (around 20 million) have acute severe obstetric complications, including haemorrhage.1,2 The first 24 hours postpartum, and the first week after labour, represent the main periods with the highest chances of mortality. The most evident postpartum complication is haemorrhage, which is the leading cause of maternal mortality in developing countries, accounting for 27% of all maternal deaths that occur worldwide.3
As Vlassoff et al.4 wrote: “Of the three types of haemorrhage—antepartum, intrapartum and postpartum—the postpartum type is by far the most important, accounting for 73% of all hemorrhage cases.”
Primary postpartum haemorrhage (PPH) is formally defined as the loss of at least 500 mL of blood after a vaginal birth, or at least 1,000 mL of blood after a Caesarean section within 24 hours of delivery, or any blood loss that may lead to hemodynamic instability.5
Postpartum complications are substantially influenced by multiple factors and variables, which range from socioeconomic status to the level of patient education, and access to proper healthcare and pregnancy follow-up, reaching to as late as the mode of delivery. Each risk factor can be linked directly to one of the established aetiologies of PPH, the four Ts: tone: uterine atony; tissue: retained products; trauma: uterine or vaginal injuries; and thrombin: bleeding disorders. A low socioeconomic status, illiteracy, and poor access to healthcare can lead to lack of antenatal care visits, which in turn leads to unnoticed antenatal problems like hypertension, which can predispose to uterine atony. In developing countries, an estimated 70% of females do not receive postpartum care, and some 60–80% of maternal deaths occur during this time period.2
To be able to identify these risk factors is to be able to prevent the morbidities and mortalities related to them. In Egypt specifically, according to demographic and health surveys, maternal mortality ratios were reduced from 84 to 52 deaths per 100,000 live births between 2000–2013.4 On a more specific note, data from this source conclude that the percentage of maternal deaths attributable to PPH declined from 34% in 2000 to 20% in 2013.4
AIM AND OBJECTIVES
The aim was to study the incidence and aetiology of PPH and their indices through measuring the incidence of postpartum haemorrhage after vaginal delivery in Kasr Al Ainy University Hospital, Cairo, Egypt, and determining the most common risk factors and aetiologies of postpartum haemorrhage in Kasr Al Ainy University Hospital.
Study Design
The authors conducted a cross-sectional study of postpartum haemorrhage after vaginal delivery in Kasr Al Ainy University Hospital, from the 1st November 2019. Postpartum haemorrhage is defined as blood loss exceeding 500 mL following vaginal delivery.
Study Setting
The study was carried out in the Obstetrics and Gynecology Emergency Department and the Postpartum Ward in Kasr Al Ainy University Hospital between 1st November 2019–15th February 2020.
The purposive selection of this hospital was based on its characteristics of being a large referral teaching hospital in the public sector with qualified health professionals, and a high caseload to mirror the population as best as possible. It is the main referral and teaching tertiary hospital in Greater Cairo, and is affiliated with the Faculty of Medicine at Cairo University.
Study Sample
In Kasr Al Ainy, the total number of vaginal deliveries in 2018 was 7,605, with an average of 20.8 deliveries per day. Therefore, the number of deliveries throughout the 106 days of data collection in the period from 1st November 2019–15th February 2020 was estimated to reach approximately 2,204.
Single population proportion formula was used to determine the sample size with the following assumptions: a confidence level of 95%, a margin of error of 5%, and a calculated global incidence of PPH after vaginal delivery of 10.8%.6 The sample size was n=139, which was then sampled using non-probability purposive sampling.
Inclusion Criteria
Inclusion criteria of this research included vaginal delivery with any presentation and any gestational age (preterm, term, post-term), multi-foetal pregnancy, vaginal birth after Caesarean section, live or still birth, and coagulopathies.
Exclusion Criteria
Exclusion criteria included performed Caesarean sections, abortion, and patients presenting to the emergency department with postpartum haemorrhage who gave birth at another hospital.
METHODOLOGY
Ethical Approval and Consent
The study protocol was approved by Cairo University’s ethical committee and review board. All participating patients provided informed consent for the collection of data.
Data Collection
The research team was responsible for carrying out the data collection, with the help of the attending residents, in a retrospective manner. Data collectors undertook a daily review of all admissions to labour, delivery, postpartum, and the emergency department to identify all eligible patients.
Patients’ charts were reviewed to retrieve the diagnosis of primary PPH. The amount of bleeding, if present, was estimated visually, as per World Health Organization (WHO) recommendations,2 and clinically2 (change in vital signs by >15% or heart rate ≥110 beats/minute, blood pressure ≤85/45 mmHg, O2 saturation <95%; California Maternal Quality Care Collaborative [CMQCC] staging system) by the resident to determine whether it was within normal limits, or classified as postpartum haemorrhage. Table 1 used data collected from the patients, using an assisted questionnaire translated to Arabic.7
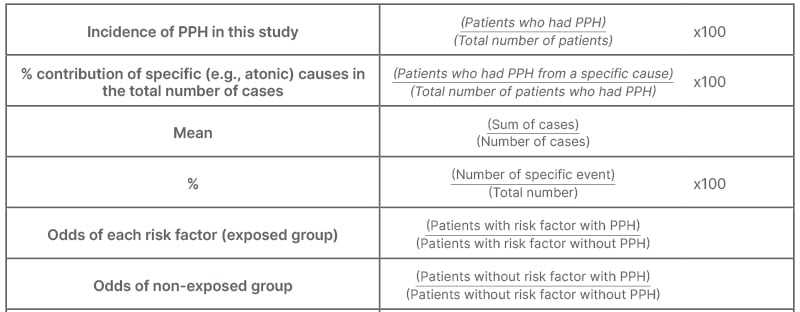
Table 1: Incidence of primary postpartum haemorrhage in this study.
PPH: primary postpartum haemorrhage.
DATA ANALYSIS
This study is a multivariate, cross-sectional study. Relative and absolute risks could not be calculated because of the multiple variables at place that can co-occur simultaneously or separately.
Confidence interval (CI) of data analysis was specified at 95%, making the margin of error (p=0.05) and its critical value determined to be 1.96, which is traditionally chosen for medical studies with p=0.05.8 The authors used a sample size for a single proportion formula calculator to calculate the necessary sample size.9 “This calculator uses the following formula for the sample size n: n=N*X / (X+N–1) where X=Zα/22 *p*(1-p)/MOE2, and Zα/2 is the critical value of the normal distribution at α/2 (e.g., for CI of 95%, α is 0.05 and the critical value is 1.96), MOE is the margin of error, p is the sample proportion (the global incidence of vaginal PPH is calculated to be 10.8%), and N is the population size.”9
A finite population adjustment has been applied to be the estimated number of deliveries throughout the period of the study (106 days [1st November 2019–15th February 2020], with an average of 20.8 deliveries/day; a finite population of 2,204 deliveries throughout the period of the study was determined).
RESULTS
The sample size required for the multivariate study with a CI of 95% was calculated to be at least 139 patients. This study included 554 patients in total, with the following population characteristics: mean maternal age: 26.6 years; 82.6% of all the participants presented with gestational age between 38–42 weeks; and 87.8% of the neonatal birth weight was between 2.5–4.0 kg (Table 1).
Population Characteristics of this Study
Incidence of PPH in this study: patients with PPH (45)/total number of patients (554) x100. The Incidence of PPH in this study was 8.12%.
Of all the risk factors, the most statistically significant of PPH (p<0.05) were all atonic causes, primarily prolonged labour (odds ratio [OR]: 5.10), history of previous PPH (OR: 4.25), hypertension (OR: 2.53), and lastly maternal age ≥35 years (OR: 2.29). Atony alone contributed to 67% of PPH, and atony with trauma contributed to 13% of PPH. Other aetiologies attributing to PPH were retained tissues (8%), bleeding disorders (8%), and traumatic causes (4%; Figure 1 and Figure 2).
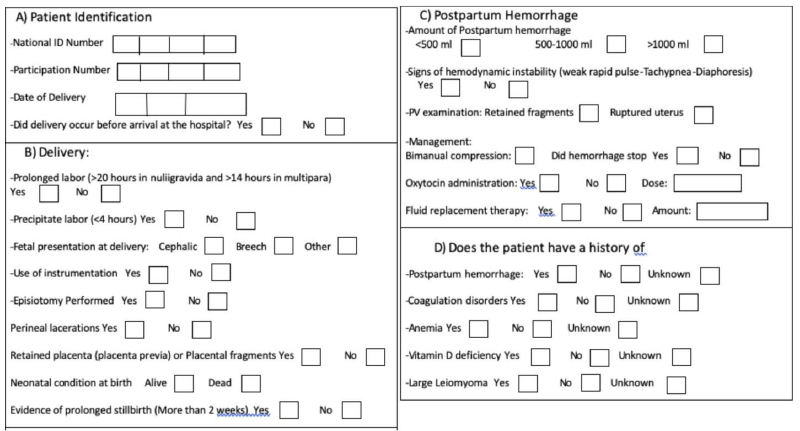
Figure 1: Contribution of major primary postpartum haemorrhage aetiologies in this study.
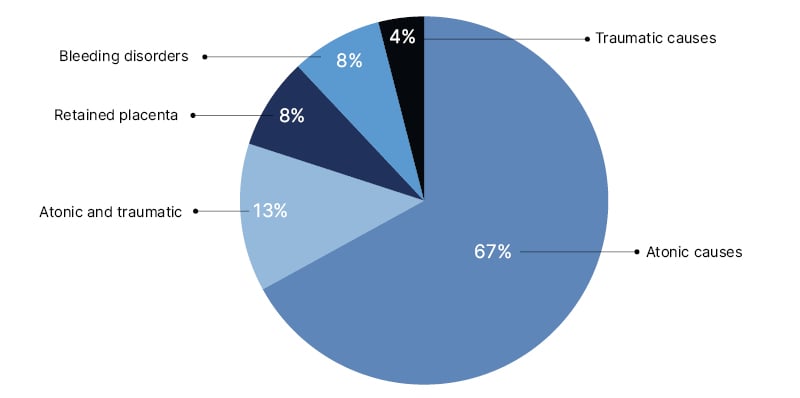
Figure 2: Major risk factors.
Major PPH causes identified in this study. Atonic causes were implicated in 67% of the cases studied; atonic and traumatic (13%); retained placenta and bleeding disorders (8%); and solely traumatic causes (4%).
PPH: primary postpartum haemorrhage.
DISCUSSION
PPH indices and risk factors differ from one country to another, and from one institution to another, depending on the facilities, skills of the doctors, and education of the public. The authors made a deliberate decision to conduct their study in a tertiary center in Egypt providing public healthcare, to be able to have a wholesome vision of risk factors and causes of PPH implicated in the mass public. To be able to identify these risk factors and aetiologies and tackle them will ultimately decrease the incidence of PPH.
PPH incidence in Kasr Al Ainy in the period of this study was 8.1%, which is lower than the calculated worldwide incidence of PPH after vaginal delivery (10.8%).6 Adding to that, it was still less than the incidence of PPH in Egypt calculated in 2013 (20%), which in turn was already less than the incidence calculated in Egypt in 2000 (34%).4 This may reflect the continuous strive to tackle risk factors of PPH, and decrease PPH incidence.
The leading risk factors identified in this study: prolonged labour, history of previous PPH, hypertension, and maternal age ≥35 years, all contribute to uterine atony as the most common aetiology of PPH. Out of all the cases studied, atony alone contributed to 67% of PPH, and atony with trauma contributed to 13% of PPH. Prolonged labour in this study was diagnosed as patients whose labour lasted over 20 hours for primigravida, and more than 14 hours in multipara, who still gave birth vaginally. Patients with prolonged labour who eventually underwent Caesarean section were excluded from the study. This highlights the urgency in tackling atony as the commonest aetiology of PPH in the authors’ region.
One noticeable aspect in this study is that bleeding disorders were attributed to 8% of the cases of PPH. Compared with the worldwide percentage of bleeding disorders causing 3% of PPH cases,10 this seems to be quite high. This can be linked to the fact that with few antenatal care visits, females with bleeding disorders are neither diagnosed, nor adequately treated before giving birth. This highlights the weight of lack of antenatal care visits as a risk factor to PPH, and provides insight to how risk factors proposed attribute to aetiologies of PPH.
The authors chose Kasr Al Ainy specifically because it is one of the largest tertiary centres in Egypt, and offers public healthcare. To avoid the bias of the tertiary center receiving referred cases, the authors excluded the patients who gave birth somewhere else and presented with established PPH. They were also able to surpass the sample size calculated (n=139), and reached 554 participants, further minimising the margin of error. On the other hand, it being the largest tertiary center might be at the advantage of having the best trained residents to deal with obstetric complications, and may not, therefore, reflect the true incidence of PHH in Egypt. However, by pointing out the most statistically significant risk factors (p<0.05) with the highest OR, those risk factors are likely be the most significant ones in other areas in Egypt and many more developing countries. With their identification, appraisal of ways to overcome these risk factors will decrease the incidence of PPH. The authors also compared their results and OR with other studies done elsewhere to test the relevance of their data.
Looking at similar studies conducted in different parts of the world, Africa had the lion’s share of PPH compared with other continents, with an incidence of 25.7%. Second was North America with PPH incidence of 13.1%, then Europe with 12.7%, Asia 8.5%, South America 8.2%, and Australia 7.2%.6
Even though, at first glance, those values can be shocking, one explanation of these variabilities can be attributed to the difference in the methodology of the studies conducted. Studies that were conducted at tertiary hospitals gave a higher incidence than elsewhere due to the referrals received.
With numerous studies conducted in different demographic areas, one may expect that risk factors would differ from one place to another. However, many studies identified the same risk factors obtained in this study as being the most significant in causing PPH.11-16 Remarkably, the OR obtained from said studies showed comparable results to the OR derived from the authors’ study. This finding serves as a valuable counterbalance to the potential bias associated with this study being conducted in a tertiary centre, with well-trained residents and greater access to interventions.
On the other hand, some studies proposed other risk factors contributing more evidently to PPH, which the authors did not observe in their study: macrosomia,17,18 use of labour induction or augmentation,16,17 and multi-foetal gestation.18,19
Thus, even though learning how to tackle each risk factor and adopting the recommendations would decrease PPH worldwide, it is still important to identify which risk factors play the biggest role in each demographic area.
STRENGTHS AND LIMITATIONS
Conducting the study in Kasr Al Ainy University Hospital, as one of the biggest tertiary centres in Egypt, meant that the authors had an extensive pool of patients. This helped a lot in exceeding the statistically suggested sample, and obtaining a more accurate presentation of the incidences and ORs of the risk factor. This strengthens the study’s statistical significance, and enriches the authors’ knowledge of the risk factors proposed, hence facilitating the confidence in adhering to the proposed recommendations.
Records were kept, albeit on paper, and the authors were able to identify the study sample in accordance with the inclusion and exclusion criteria; this helped in the follow-up of blood loss and management.
On the other hand, the authors were aiming to continue data collection for a longer period to obtain even more inclusive data, but this came to a halt due to the emergence of the COVID-19 pandemic. Adding to that, with the new emerging studies on the effect of previously contracting COVID-19 with haematological diseases, including coagulopathies, the authors deemed it best to avoid resumption of data collection with the introduction of a new variant in the risk factors.
Another limitation faced was the unavailability of digital records of the patients. To manually go through patient’s files and documents with the high caseload put a strain on the authors’ timeframe, and decreased the efficiency of the study.
CONCLUSION
The incidence of PPH in Kasr Al Ainy is 8.1%, which, even though is less than the incidence studied in 2013 in Egypt,4 and less than the worldwide incidence of PPH,6 is still high. To decrease this incidence, a review of the most statistically significant risk factors was vital. Atonic causes of postpartum dominated the risk factors, most significant of which are prolonged labour, history of previous PPH, hypertension, and advanced maternal age ≥35 years.
RECOMMENDATIONS
To tackle the risk factors as early as possible, antenatal care and antenatal care visits with health education to mothers are of critical importance. This can early on identify high risk patients; stabilise any current comorbidities, including hypertension or coagulopathies; and track the progression of the pregnancy.
Another way is to prevent prolonged labour, which can be done through timely follow-up of the stages of labour of the patient, defining high risk patients, and initiating early intervention when required.
Adherence to active management of the third stage of labour, including routine administration of oxytocin, which can prevent atony; clamping and cutting the umbilical cord immediately after delivery; and controlled cord traction can prevent bleeding.20
Other measures that can be adopted are avoiding injurious instrumental deliveries, immediate repair of any vaginal or perineal tears, and making sure there are no products of conception left.







