Abstract
Objective: To compare the immediate perinatal outcome of females with maternal near-miss (MNM) morbidity and those without near-miss morbidity in Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
Methods: A case-control study was conducted at MTRH. Near-miss cases were identified using World Health Organization (WHO) criteria for near-miss. A consecutive sampling technique was applied to obtain a total of 45 cases and 225 controls. Determinants of near-miss were assessed using a binary logistic regression model. Perinatal outcomes were compared between the near-miss and control.
Results: Severe maternal outcome ratio was 11.4 per 1,000 live births, the MNM ratio was 10.4 per 1,000 live births (95% confidence interval [CI]:7.6–13.9), and MNM mortality ratio was 11.2. The most common condition associated with near-miss was haematological or coagulation dysfunction (64%). Hypertension was the leading underlying cause of near-miss (35%). Factors associated with reduced odds of near-miss were employment (odds ratio: 0.12; 95% CI: 0.03–0.42) and awareness of danger signs (odds ratio: 0.41; 95% CI: 0.19–0.91). Most babies of the near-miss cases were born alive (76%), with median appearance, pulse, grimace, activity, respiration (Apgar) score of 9/10; stillbirth rate was 22%; and median birth weight was 2,700 g. This was similar to the control group with live birth at 77%, a median Apgar score of 9/10, and stillbirth of 23%. There was no statistically significant difference in perinatal outcome between cases and control.
Conclusion: MNM indicators are comparable to the world. The determinants of near-miss are unemployment and lack of awareness of danger signs. There was no difference in perinatal outcome between the cases and control.
Key Points
1. The identification of maternal near-miss is important for preventing complications that lead to death and for highlighting opportunities to avoid similar cases in the future.2. This case-control study examined the maternal near-miss indicators among pregnant patients at a Kenyan Hospital, finding that the determinants of near-miss were unemployment and lack of awareness of danger signs.
3. Education on danger signs should be encouraged, and peripheral facilities should be equipped with theatre and personnel to reduce referral and offer timely intervention.
INTRODUCTION
Improving maternal health has been a major concern worldwide. This is evident by maternal health being included in the Millennium Development Goals, with the goal of reducing maternal mortality by three-quarters by 2015, and now the Sustainable Development Goals, with targets set to reduce the global maternal mortality ratio to less than 70 per 100,000 live births. It further states that no country should have maternal mortality above 140 per 100,000 live births by 2030.1
Progress on reduction of maternal mortality has been slow. Globally, the estimated maternal mortality of 2013 was 289,000, with sub-Saharan Africa accounting for 62% of this.2 Although this was a 45% reduction from 1990, this has been very far from what was set to be achieved in the Millennium Development Goals. Most of the countries, including Kenya, did not achieve the Millennium Development Goals, which expired at the end of 2015.
Reduction in maternal mortality has traditionally been used as a critical measure of maternal health, but this represents only a glimpse of the burden of maternal morbidity. For every maternal death, there are close to 100 females with severe maternal morbidity (SMM) referred to as maternal near-miss (MNM).3 Hence, relying solely on maternal mortality to assess maternal health overlooks the pregnancy continuum from normal to death. On this continuum, pregnancy, labour, or the puerperium may be classified as uncomplicated, complicated, severely complicated, life-threatening, or fatal.4 In life-threatening pregnancy-related complications, the female has one of two severe maternal outcomes: they may die (maternal deaths) or narrowly escape death (MNM cases).
MNM is defined as a female who nearly died but survived a complication that occurred during pregnancy, childbirth, or within 42 days of termination of pregnancy.5 Theoretically, these females are considered near-miss retrospectively when they survive organ dysfunction. Females who undergo a MNM have many common characteristics with those who die from the complication.5 Similar to the cases of maternal mortality, MNM cases are preventable. Thus, the identification of MNM is important for preventing complications that lead to death and for highlighting ways and opportunities to avoid similar cases in the future.
MNM approach is being used to describe local patterns of maternal mortality and morbidity, strengths and weaknesses in the referral system, and the use of clinical and other healthcare interventions. Despite its wide application, there were challenges with its use mainly due to the absence of universal criteria for the identification of cases. In 2009, a criterion for MNM identification was developed by the World Health Organization (WHO) working group for maternal health so as to standardise the detection of MNM cases. This is a two-step process. Firstly, maternal cases with potentially life-threatening conditions such as SMM, which may or may not be near-miss cases (e.g., specific complications such as severe pre-eclampsia and/or critical interventions such as blood transfusion), are identified. Secondly, identification of near-miss cases based on organ system dysfunction and organ dysfunction proxies, including clinical, laboratory, and management criteria.6
In Kenya, MNM morbidity review is considered one of the many strategies to tackle high maternal mortality. The national maternal and perinatal death surveillance and response (MPDSR) committee recommend a review of MNM cases in order to reduce the maternal mortality rate to less than 200 per 100,000 live births by 2030.
Problem Statement
Inquiries into maternal healthcare have for a long time used maternal death as the starting point of investigations. Death is the worst maternal adverse event in pregnancy and viewing the circumstances around the death may reveal some avoidable health factors. However, despite the high maternal mortality ratios, in many countries with resource-poor settings, maternal deaths are rare in absolute numbers per centre. This does not allow detailed quantification of the associated risk factors and determinants that are locally important. In the last 20 years, the idea of MNM has been explored in maternal health as an adjunct to maternal death confidential enquiries. Among other advantages, near-miss cases occur more frequently than maternal deaths and can directly inform on problems and obstacles that had to be overcome during the process of healthcare, providing more robust conclusions and rapid reporting on maternal care issues.7
Study Objective
To determine the MNM indicators among females who are pregnant seeking healthcare at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
METHODS
Study Setting
The study was carried out at the maternity wing, gynaecology ward, cardiac unit, intensive care unit, high dependency unit, and renal unit of MTRH.
Study Design
This was a case-control study of females who nearly died but survived a complication that occurred during pregnancy, childbirth, or within 42 days of termination of pregnancy (near-miss). The control group was females with similar conditions causing a near-miss but does not fulfill the near-miss criteria. For each case of near-miss, four matched controls were selected. The age, gestation age of pregnancy, parity, and condition causing near-miss were considered during the match selection.
Study Population
The study population was females who were pregnant, those within 42 days of termination of pregnancy, and babies delivered to these mothers seeking healthcare at the MTRH.
Sample Size
The exposure rate among the controls was 47%. Hence, with 45 cases and 180 controls (based on a ratio of four controls for every case), a total of 225 participants were recruited for the study.
The exposure rates were calculated from records of prior cases in the hospital records. The indirect causes of near-miss were deduced from the three delays model, which includes decision making, reaching the facility, and receiving adequate care.
Sampling Technique and Study Procedure
The sample population included all females presenting to the hospital seeking healthcare during pregnancy, labour, delivery, and/or within 42 days after delivery or termination of pregnancy. Once any of these females were discharged from the maternity wards, they were screened for the presence of any SMM or potential life-threatening and a severe maternal outcome like MNM. The identification of SMM was based on diagnostic categories such as obstetrical haemorrhage, hypertensive disorders, sepsis or severe systemic infection, uterine rupture, early pregnancy complications, and/or other indirect causes. The females who had SMM were then screened as per WHO criteria for near-miss and those who qualified were included in the study.
Once a near-miss was identified, matched controls were then selected from the population of females with potentially life-threatening conditions in the wards. In order to reduce bias as a result of chance, four controls per near-miss were included.
Data Management and Statistical Analysis
Data was collected using a structured questionnaire. Data analysis was conducted using software for statistical computing called R.8 Categorical variables, such as level of education, marital status, source of income, residence, and possession of health insurance, were summarised using frequencies and the corresponding percentages. Continuous variables, such as gestational age, and discrete variables, such as the number of pregnancies and number of births, were summarised using the mean and the corresponding standard deviation.
Comparison of categorical variables by cases and controls was performed using Fisher’s exact test due to violation of Pearson’s chi-squared assumptions for most categorical variables. Continuous and discrete variables were compared using two-sample Wilcoxon rank-sum test and independent samples t-test. The authors reported the associated p values.
Determinants of near-miss were assessed using a binary logistic regression model. Factors that were established to be associated with near-miss in the bivariate analysis were all included in the multivariate logistic regression model. The authors reported the odds ratios (OR) and the corresponding 95% confidence intervals (CI).
Ethical Considerations
Approval to conduct the study was sought and obtained from the institutional research and ethics committee. Permission to conduct the study was sought from MTRH. Informed consent from the participants and guardians for those less than 18 years. Consent was obtained for minors (under the age of 18 years).
RESULTS
The proportions of participants with a level of income more than 6,000 KSH were similar for the cases and the controls (11.1% versus 16.1%; p=0.491). The MNM cases were significantly less likely to have health insurance than the controls (15.6% versus 31.1%; p=0.042).
The female’s reproductive and obstetrical information on the current pregnancy was collected. The median gestational age was similar for the cases and the controls: 38 weeks (interquartile range [IQR]: 36–38 weeks) versus 38 weeks (IQR: 36–39 weeks); p=0.461. There was no evidence from the data on the difference in the modes of delivery between the two groups (p>0.05). There was borderline significance in the proportion who attended the antenatal clinic between the cases and the controls (84.4% versus 93.9%; p=0.052).
A significantly lower proportion of the cases were aware of the danger signs of pregnancy compared with the controls (26.7% versus 48.3%; p=0.011). The proportion admitted to the hospital during the current pregnancy among the cases and among the controls were similar (26.7% versus 18.3%; p=0.216). Similarly, the proportion who had a birth plan among the cases and among the controls were also similar (51.1% versus 64.2%; p=0.124).
Female’s Reproductive and Obstetrical Information on Current Pregnancy
Data on the past obstetric history was collected. The findings demonstrated that a significantly higher proportion of participants among the cases had an interpregnancy period of more than 3 years (46.7% versus 14.9%; p<0.001).
There was no difference in the proportion of participants who had a history of complications in the previous pregnancy among the cases and among the controls (53.3% versus 61.9%; p=0.414). However, among the participants who had a history of complications in pregnancy, the proportion of participants who had experienced stillbirths in the MNM cases was significantly higher than that observed among the controls (37.5% versus 7.2%; p=0.004).
History of chronic illnesses was reported by a higher proportion among the cases (35.6%) relative to the controls (29.1%); however, there was insufficient evidence to link the history of chronic illnesses with near-miss (p=0.468). The proportion of participants who reported specific chronic illnesses among the cases and among the controls was not statistically significantly different (p>0.05).
Overall, 77.5% of the children were born alive. This represented 76.3% among the cases, and 77.8% among the controls. The fresh and macerated stillbirths accounted for 22.5%, with 23.7% among the cases, and 24.2% among the controls. This was not statistically different between the groups (p=0.831).
The median birth weights were similar for the cases and the controls (median birth weight: 2,700 g [IQR: 2,000–3,050 g] versus 2,850 g [IQR: 2,600–3,100 g]; p=0.068). Similarly, the median Apgar scores were similar for the MNM cases and the controls (9.0 [IQR: 2.0–10.0] versus 9.0 [IQR: 7.8–10.0]; p=0.429).
The proportion of children admitted to the newborn unit among the cases and the controls (46.4% versus 44.8%; p>0.999), as well as the proportion of children alive and discharged or alive by Day 7 among the cases and the controls (85.7% versus 93.1%; p=0.249) were similar.
The results show that most of the participants who were diagnosed with near-miss presented with haematological or coagulation dysfunction (64.4%), followed by cardiovascular dysfunction (24.4%). The underlying cause of near-miss was mainly hypertensive disorders (35.6%), followed by medical/surgical diseases (28.9%).
DISCUSSION
Perinatal Outcome
There was no difference in birth weight, stillbirth, admission to the newborn unit, Apgar score, and condition on the discharge of the babies born between the cases and control.
This finding was similar to a study in Brazil that showed no difference in Apgar score at 5 minutes and birth weight. This finding was different from a study in Nigeria that found near-miss was associated with stillbirth, low birth weight, and postmature pregnancy.9,10 This study was different from the authors’ study in that it used unmatched controls, meaning their controls had normal pregnancy and hence could differentiate from the MNM cases. In the authors’ study, the controls were matched with the cases hence similar underlying pathology, which could have contributed to a similar outcome.
It was noted that the active phase of labour taking more than 6 hours was associated with near-miss compared with controls. Most of the near-miss came to the hospital as referrals. The third delay, which is referral from one facility to the final facility, of more than 2 hours was found to be significantly higher in the near-miss group relative to the control. The most common reason for referral was the lack of personnel. It was also found that those who made decisions within 30 minutes of symptom onset were more likely to be near-miss.
Although there is no near-miss study that looks at the duration of labour as a risk factor, prolonged labour is associated with several adverse maternal outcomes (e.g., postpartum haemorrhage, uterine rapture, puerperal sepsis, and caesarian section), and these conditions could cause near-miss.11
Several studies have linked near-miss to delays. Most attribute to all the delays, namely delay in decision making, delay in arriving at the hospital, and delay in attaining medical care due to either lack of personnel or poorly equipped hospitals leading to referral to a more equipped hospital.12-14 Most hospitals in developing countries are under-resourced, leading to delays in initiating treatment and offering timely referrals.15 Seeking care from a facility that is ill-equipped to give emergency obstetric care contributes to significant delay even after reaching the health facility. These factors were reported as significant contributors of delay in several studies.16 As a matter of fact, these non-functional health facilities are physically accessible but act as physical obstacles for females who are pregnant in accessing a functioning health facility in time. From the authors’ study, third delay was associated with near-miss, especially among those who sought treatment in a health facility with no personnel or lack of facility to handle the emergency. Those who took more than 2 hours to reach the final destination were associated with near-miss. This is true because almost all government facilities in Uasin Gishu County, Eldoret, Kenya, can only offer basic obstetric care, and this leads to delays in offering care to the females at risk of developing a near-miss.
Most of the patients with a near-miss were referred to or came to the hospital with complications already. Only two of the complications developed in the hospital. This is in keeping with another study in a tertiary hospital in this region, which showed that most onsets of near-miss complications happen in referring facilities.15 The complexity of care and treatment provided to patients in the obstetric ward ranges from basic to intensive care and thus the level of health facilities is different too.17
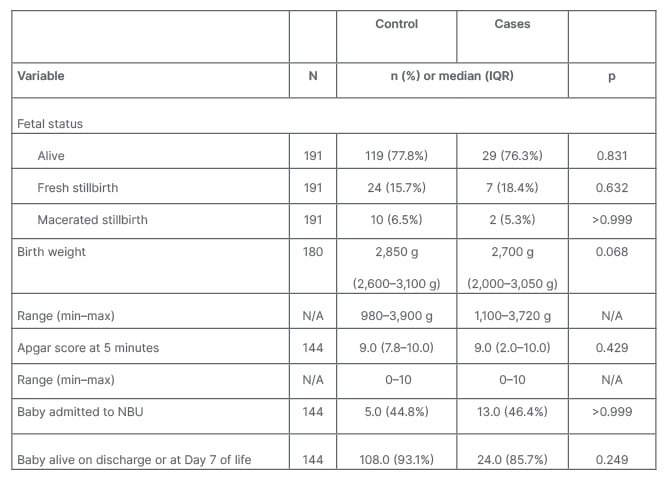
Table 1: Perinatal outcomes.
IQR: interquartile range; max: maximum; min: minimum; N/A: not applicable; NBU: newborn units.
Causes of Near-Miss
The results show that most of the participants who were diagnosed with near-miss presented with haematological or coagulation dysfunction (64.4%), cardiovascular dysfunction (24.4%), neurological dysfunction (15%), renal dysfunction (13%), and hepatic and respiratory dysfunction (8%). The underlying cause of near-miss was mainly hypertensive disorders (35.6%), followed by medical/surgical diseases (28.9%), and obstetric haemorrhage (17%).
These findings are similar to a study in Malaysia,18 which found haematological or coagulation dysfunction to be the most common cause of organ dysfunction. The underlying cause of near-miss was hypertensive disorder, and this is similar to studies carried out in the region.15,19 The similarity is also observed in complications caused by medical/surgical diseases, especially sepsis.19 Obstetric haemorrhage came third, which is also similar to other studies. It could be due to the widespread use of protocols for the management of postpartum haemorrhage even at the lower-level facilities. Direct causes of near-miss were different compared with a study in Kenyatta National Hospital, Nairobi, Kenya, which found that haemorrhage and hypertension were the most common diseases causing near-miss.20 The difference could be due to changing times. In the last decade, there has been a lot of advocacy to reduce postpartum haemorrhage by use of uterotonic drugs. Indeed, a recent study showed up to 95% of delivering females received uterotonic drugs as management of the third stage, which could explain the reduction.21
CONCLUSION
There was no difference in perinatal outcome between near-miss cases and the controls.
RECOMMENDATIONS
- Health education should be encouraged on the danger signs, during antenatal clinic visits, as many cases of near-miss demonstrated a lack of awareness of danger signs.
- Equipping the peripheral facilities with theatre and personnel to reduce referral and offer timely intervention. The most common reason for referring was lack of personnel and expertise.
STUDY LIMITATIONS
This study is a hospital-based study and its findings may not be generalised. MTRH is the only government facility offering comprehensive obstetric care within Uasin Gishu County. Therefore, the large concentration of pregnant females with previous comorbidities and obstetric complications might have overestimated the indicators. This was a case-control study, hence could not be used to estimate the incidence of near-miss.








