Abstract
Objective: To determine the fetomaternal outcomes of low-risk females presenting with perceived reduced fetal movements at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
Methods: This was a cross-sectional study among 133 females of gestation between 34–41 weeks presenting with a perception of reduced fetal movement, who were consecutively recruited. Pearson χ2 and Fischer’s exact tests of association were used to test the association between the non-stress test (NST) findings, biophysical profile (BPP) scores, and fetomaternal outcomes, where p≤0.05 was considered statistically significant.
Results: A reactive NST finding was seen in 88 (66.2%) participants with 104 (78.2%) of all participants enrolled having a normal BPP score. Active management of the current pregnancy was offered to 89 (66.9%) of the participants, and 81 (60.9%) of the females had a vaginal delivery. Three quarters (76.7%) of the newborns had a 5-minute appearance, pulse, grimace, activity, and respiration (APGAR) score ≥7, 18 (13.5%) were resuscitated, 13 (9.8%) were admitted to the newborn unit, and four (3%) fresh stillbirths were noted. Both NST (p<0.001) and BPP (p<0.001) were good predictors of a 5-minute APGAR score ≥7, but poorly (p=0.086) predicted resuscitation. There was a statistically significant association between the NST findings and admission to newborn unit (p=0.034).
Conclusion: A reactive NST is a good predictor of a 5-minute APGAR score greater than 7, and is associated with a reduced likelihood of both admission to the newborn unit and newborn resuscitation. Both reactive NST and normal BPP are good predictors of vaginal delivery as opposed to Caesarean delivery.
Key Points
1. The findings of this study will influence the diagnosis and management of reduced fetal movements in low-risk pregnancies among expectant females attending both resource-rich and resource-limited public healthcare settings in Kenya.
2. This study therefore aimed to establish the fetomaternal outcomes following a diagnosis of reduced fetal movements among low-risk expectant mothers at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. Furthermore, the study compared two commonly used diagnostic tools, namely the non-stress test and biophysical profile.
3. A non-stress test can be used in place of biophysical profile in low-resource clinical settings, where ultrasound services are not readily accessible, as a good predictor of immediate fetal outcomes among low-risk expectant females with perceived reduced fetal movements.
BACKGROUND
Fetal movements are defined as any discrete kick, flutter, swish, or roll, first perceived between 16–18 weeks in multiparous females and 20–22 weeks among primiparous females, a period long before fetal viability in the current set-up. Also referred to as ‘quickening’, there is considerable variation in the perception of the first movements among expectant females, depending on the parity, as alluded in the above definition. There is no universal definition of reduced fetal movements (RFM); however, the majority of the international bodies, journals, and institutions agree on less than 10 movements in 12 hours,1,2 concurring with the 1976 definition of Pearson and Weaver who developed the Cardiff ‘count-to-ten’ kick chart.3 In that study, the authors noted that intrauterine death was preceded by reduction in perception of fetal movements in the previous 3–4 days, followed by complete cessation of perception of the movements 12–48 hours before eventual fetal demise.3 Soufizadeh et al.4 also reported that while RFM was a predictor of adverse fetal outcomes, perception of normal movements is especially useful to the mother as it allays fears of imminent fetal death. For the obstetrician, it offers assurance of good fetal wellbeing in case postponement of delivery is needed to allow for lung maturity.4
For the expectant female, RFM is a major cause of concern. Consequently, reduced fetal movements have been shown to be a major indication for hospitalisation, at the detriment of overwhelming the facilities, and crucially, especially in the third world, the already low numbers of the healthcare workers. Despite reduced fetal movements being a common problem among expectant females, the clinical significance of a history of reduced fetal movements remains unclear, and assessment and management of these pregnancies is still controversial.5
RFM is a common reason for admission of expectant females in many reproductive health facilities in Kenya. The majority of the expectant mothers with this complaint are usually apprehensive and anxious to find out about the wellbeing of their babies. There is limited correlation between the surveillance tools used in the evaluation of reduced fetal movements and pregnancy outcomes in many public health facilities, such as Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. In addition, the magnitude of undesirable pregnancy outcomes related to reduced fetal movements in low-risk pregnancies has not been adequately documented in Western Kenya. This creates the need for a local study to provide empirical evidence of reduced fetal movements in low-risk pregnancies and the resulting pregnancy outcomes. This study therefore aimed to establish the fetal and maternal outcomes following a diagnosis of reduced fetal movements among low-risk expectant mothers at MTRH. Furthermore, the study compared two commonly used diagnostic tools, namely the non-stress test (NST) and biophysical profile (BPP). Would the NST alone have the same evaluation benefit for these cohort of patients? The findings of this study will influence the diagnosis and management of reduced fetal movements in low-risk pregnancies among expectant females attending both resource-rich and resource-limited public healthcare settings in Kenya.
STUDY OBJECTIVE
The objective was to describe the fetal and maternal outcomes in low-risk females presenting with perceived reduced fetal movements at MTRH.
METHODS
Study Design
This study adopted a descriptive, cross-sectional study design among low-risk expectant females with reduced fetal movements (Figure 1). This was deemed appropriate owing to the small numbers left after excluding high-risk pregnancies, which make the bulk of the females presenting with perceived reduced fetal movements.
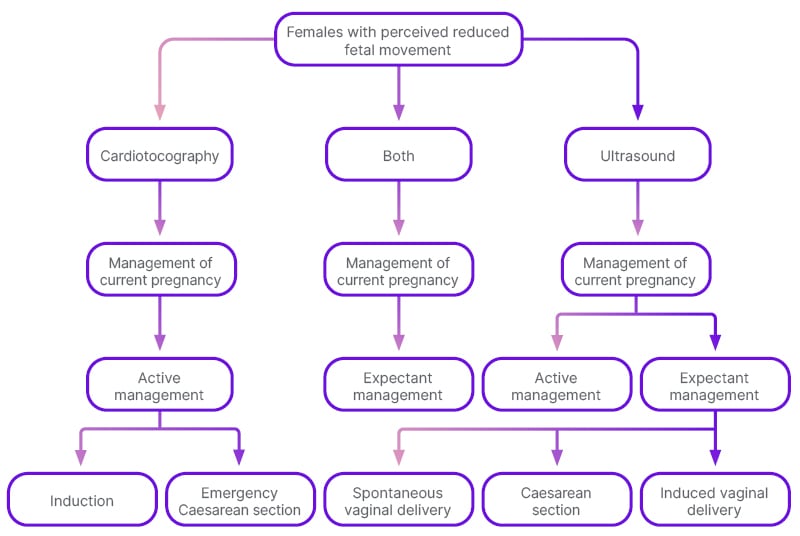
Figure 1: Study flow chart.
Study Setting
The study was conducted at MTRH’s Riley Mother and Baby Hospital (RMBH) labour ward and the newborn unit (NBU).
Study Period
This study was carried for a period of 12 months between June 2019–May 2020.
Study Population
All low-risk expectant females with perceived reduced fetal movements seeking care at MTRH’s maternity unit and their newborns.
Inclusion Criteria
All females with over 34 weeks’ gestation and not more than 41 weeks with complains of reduced fetal movement were included.
Exclusion Criteria
Patients who were in labour and those who declined consent were excluded.
Sampling Technique
Potential study participants were consecutively sampled until the desired sample size was achieved.
Study Procedure
All expectant females who met the eligibility criteria between 27th June 2019–26th June 2020 were approached and told about study objectives. After they consented, they were subjected to both NST and ultrasound examination so as to compute the BPP. The ultrasound was performed by the radiologist on duty or the maternal-fetal medicine consultant. The NST results were computed as either reactive or non-reactive, as per the clinical management guidelines of MTRH’s maternity unit. The BPP was then computed by summing the scores from both the NST and obstetric ultrasound. Following the BPP scoring, participants were managed either actively or expectantly, as per the hospital guidelines. Participants’ sociodemographic and clinical data were collected and documented using an interviewer administered questionnaire. Fetal and maternal outcomes following delivery were obtained by reviewing medical records without meeting the study participant, within 24 hours. These post-delivery outcomes of interest among females with reduced fetal movements were: gestational age, mode of delivery, appearance, pulse, grimace, activity, and respiration (APGAR) score at 5 minutes, need for resuscitation, admission to NBU, or occurrence of fresh stillbirth.
Data Management and Analysis
A pilot study on 10% of the estimated sample size was carried out at RMBH. The questionnaire was tested for its clarity, understandability, length, and completeness. Culturally sensitive questions that needed to be changed before the main study were addressed.
Data were collected using a structured questionnaire. Primary data collected included sociodemographic characteristics. Secondary data included results of evaluations and interventions offered to the participants, as well as the maternal and fetal outcomes. The questionnaires were checked for completeness at the end of each data collection session. Double data entry was then performed to ensure completeness of the data, as well as its accuracy and reliability using the statistical package for social sciences (SPSS) version 24 software (IBM, Armonk, New York, USA). Data were maintained strictly confidential and access was restricted only to the principal investigator and the research assistants. Questionnaires were kept in safe data cabinets with lock and key. The computer databases were password protected to restrict access from unauthorised individuals.
Descriptive statistical techniques adopting measures of central tendency and dispersion, such as the mean, interquartile range, and the standard deviation, were used to summarise continuous variables. Categorical variables were summarised as frequencies and the corresponding percentages. Bivariate analysis was carried out to check for association between dependent and independent variables where Pearson’s χ2 and Fisher’s exact tests were used. Variables that were found to be statistically significant at bivariate level were subjected to multivariate logistic regression, and results reported as adjusted odds ratio with a 95% confidence interval. The findings were presented in the form of tables.
Ethical Consideration
Ethical approval to conduct the study was obtained from the Institutional Research Ethics Committee (IREC) at the MTRH and Moi University School of Medicine, Eldoret, Kenya.
RESULTS
This study enrolled 152 expectant females, five of whom did not have cardiotocographic findings, while 14 did not get an obstetric ultrasound done. They were therefore dropped from the final analysis, leaving 133 females with a mean age of 27.8 (±5.1) years. Almost all (98.5%; n=131) the patients had attended antenatal clinic during the course of their pregnancy, and 85 (64.9%) were multiparous, with the rest being primiparous.
Results of Evaluations and Interventions Given to Females Who Present at MTRH with Perceived Reduced Fetal Movements
Among the participants, 85 out of 133 (63.9%) received active management of the current pregnancy, while the remaining 48 (36.1%) were offered expectant management of their current pregnancy. Out of the 133 participants, 88 (66.1%) had a reactive NST, with the remaining 45 (33.8%) recording a non-reactive NST. When the mode of management was compared based on cardiotocographic findings, it was noted that 48 out of the 88 (54.5%) participants with a reactive NST finding received active management, compared to 37 out of 45 (82.2%) of those with a non-reactive NST finding. When BPP scores were categorised as abnormal (≤4), equivocal (6), or normal (>6), 17 out of 19 (89.5%) participants with an abnormal BPP received active management. All the 10 participants (100.0%) with an equivocal BPP received active management, whereas only 58 out of the 104 (55.8%) with a normal BPP received active management. There was a statistically significant relationship between NST findings (p=0.016), BPP score (p=0.001), and management of the current pregnancy (Table 1).
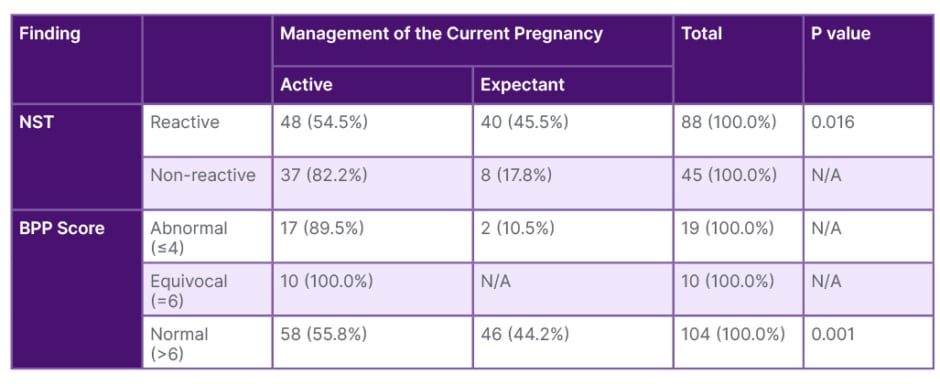
Table 1: Comparison between reduced fetal movements evaluations and management of current pregnancy.
BPP: biophysical profile; N/A: not applicable; NST: non-stress test.
Fetal Outcomes in Females Presenting with Perceived Reduced Fetal Movements at MTRH
When NST and BPP findings were compared to 5-minute APGAR score, 76 out of the 88 (86.4%) participants with a reactive NST finding had neonates with a 5-minute APGAR score ≥7, compared to 26 out of the 45 (57.8%) participants who had a non-reactive NST finding and neonates with a 5-minute APGAR score of >7. It was found that 89 out of the 104 participants (85.6%) with a BPP score of 8 or 10 (normal) gave birth to neonates with a 5-minute APGAR score >7. In comparison, only six out of the 19 participants (31.6%) with a BPP score of ≤4 (abnormal) had neonates with a 5-minute APGAR score of >7. This relationship between NST findings, BPP score, and 5-minute APGAR score was found to be statistically significant (p<0.001), as shown in Table 2.
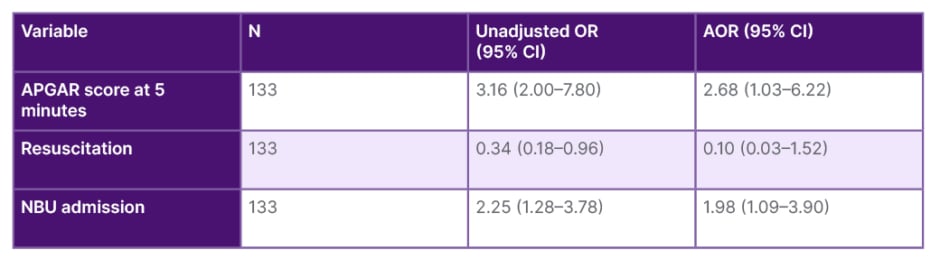
Table 2: Multivariate logistic regression association between significant variables and fetal outcomes.
AOR: adjusted odds ratio; APGAR: appearance, pulse, grimace, activity, and respiration; CI: confidence interval; NBU: newborn unit; OR: odds ratio.
There was a higher proportion of resuscitation among neonates for females with a non-reactive NST finding, with 10 out of 45 (22.5%) being resuscitated, compared to those with a reactive NST finding where only eight out of 88 (9.1%) were resuscitated. However, this relationship was not statistically significant (p=0.058). Similarly, the combined proportion of resuscitation among those neonates of participants with abnormal and equivocal BPP was higher compared to those with a normal BPP score, without any statistically significant difference (p=0.086).
In this study, eight out of 45 (17.8%) of the neonates born of participants with a non-reactive NST finding were admitted to the NBU, compared to five out of 88 (7.3%) of those born to mothers with a reactive NST finding. This relationship was found to be statistically significant (p=0.034).
In this study, three out of 45 (6.7%) neonates whose mothers had a non-reactive NST were stillbirths. When analysed against the BPP score, three out of the 19 (15.8%) neonates born of participants with an abnormal score (≤4) were stillbirths. Both NST and BPP findings were significantly (p=0.008) associated with fresh stillbirth.
Among the participants with a reactive NST finding, 78 out of the 88 (88.7%) had neonates with a birth weight of >2,500 g. However, in comparison, 33 out of the 45 (73.3%) of the participants with a non-reactive NST had neonates of <2,500 g. This relationship was found to be statistically significant (p=0.011). BPP score increased with an increase in birthweight. A higher birthweight was significantly associated with a higher BPP score (p<0.001).
Maternal Outcomes in Females Presenting with Perceived Reduced Fetal Movements in MTRH
In this study, 38 out of 85 (44.7%) of the participants who had active management of their current pregnancy had induced vaginal delivery, while 45 out of the 85 (55.3%) participants in this management category had an emergency Caesarean section. Expectant management of the current pregnancy was offered to 48 females with perceived reduced fetal movements. Of these patients, 31 (64.6%) had spontaneous vaginal delivery, followed by induced vaginal delivery in 13 out of the 48 (27.1%) participants. The least occurring mode of delivery in the expectant arm was through emergency Caesarean section, which was offered to four out of the 48 (8.3%) participants. The main indication for emergency Caesarean section was a non-reassuring fetal status at 78.7%.
Both NST and BPP were statistically associated with the mode of the management for the current pregnancy (p<0.001; Table 2 and 3).
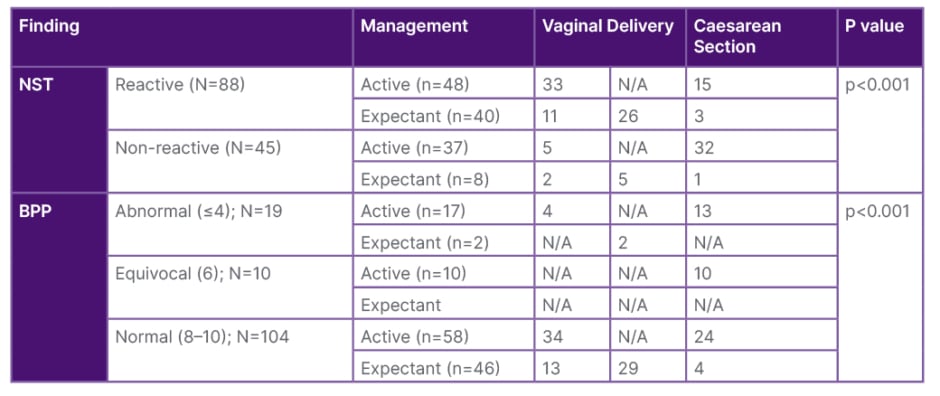
Table 3: Association between evaluations and mode of delivery.
BPP: biophysical profile; N/A: not applicable; NST: non-stress test.
DISCUSSION
In this study, 88 out of 133 (66.2%) of the participants enrolled had a reactive NST finding, compared to 45 out of 133 (33.8%) participants who had a non-reactive NST finding. This compares to findings from Saudi Arabia,6 which reported that 32.9% of the participants had a non-reactive NST finding. Contrasting findings were observed in studies reviewed from Ireland7 and Kolkata, India,8 which reported a nearly uniform finding of reactive NST among the females enrolled. In Ireland, the proportion of reactive NST findings was observed to be 94.8%,7 while in India, the authors8 reported that 98.3% of the females enrolled in the prospective study had a reactive NST finding. This higher occurrence of reactive NST finding could be attributed to early health seeking behaviour reported in Europe, as opposed to Sub-Saharan Africa, thus allowing detection of deteriorating fetal status much earlier.
Nearly equal proportions of reactive and non-reactive NST findings were noted in Dhaka, Bangladesh,9 at 49% and 51%, respectively. In Lahore-Pakistan,10 the proportion of reactive and non-reactive NST findings stood at 57.9% and 42.1%, respectively. The lowest proportion of a reactive NST finding was reported in Iran,4 at 15.3%. This was because all the females enrolled had insulin dependent diabetes, compared to this study, which excluded females with comorbidities such as diabetes and hypertension.
In this study, 104 out of 133 (78.2%) participants had a BPP score of 8 or 10, which is considered normal. In comparison, 10 out of 133 (7.5%) of participants had an abnormal (≤4) score, whereas 19 out of the 133 (14.3%) participants had an equivocal (6) BPP score. This trend was also noted in a study conducted in Iran,4 where 70.4% of the females had a normal BPP score. However, there was a higher proportion (26.1%) of equivocal BPP score with the lowest being an abnormal finding (3.5%). The differences in equivocal and abnormal findings could be attributed to the eligibility criteria adopted by the current study, which excluded high-risk females with comorbidities such as hypertensive disease in pregnancy, cardiac disease in pregnancy, and anaemia, as compared to the study conducted in Iran.
The proportion of vaginal delivery among participants with perceived reduced fetal movements enrolled in this study was 61.7% (82 out of 133 participants) with the remaining 51 out of 133 (38.3%) participants delivering via Caesarean section. This is comparable to Ireland, at 68% for vaginal delivery and 32% for Caesarean section.7 However, in Multan, Pakistan,6 the authors noted a lower (27.8%) proportion of vaginal delivery compared to Caesarean section (72.2%).
The authors’ study established that neonates of mothers with a non-reactive NST were more likely to be admitted to the NBU (17.8%), compared to those with a reactive finding (5.7%). This relationship was found to be statistically significant (p=0.034). However, no statistically significant association (p=0.058) was found between BPP finding and admission to the NBU.
CONCLUSIONS AND RECOMMENDATIONS
A reactive NST is a good predictor of a 5-minute APGAR score greater than 7, and is associated with a reduced likelihood of both admission to the NBU and occurrence of fresh stillbirth. However, it was not significantly associated with the need for neonatal resuscitation among low-risk females with perception of reduced fetal movements. Both reactive NST and normal BPP are good predictors of vaginal delivery as opposed to Caesarean delivery in low-risk females with perceived reduced fetal movements.
Recommendations
An NST can be used in place of BPP in low resource clinical settings, where ultrasound services are not readily accessible, as a good predictor of immediate fetal outcomes among low-risk expectant females with perceived RFM.
Future larger studies adopting longitudinal case-control designs should be conducted to further validate this study’s findings.







