Abstract
Background: Insertion of a post-placental intrauterine contraceptive device (PPIUCD) has been recommended by the World Health Organization (WHO) as one of the safe and effective methods of temporary contraception. In the immediate post-delivery period, females are highly driven and in need of an effective method for contraception so that child-rearing can be easy without u nintended pregnancy.
Objective: To assess the outcome of females accepting PPIUCD in terms of insertion, complications, and discontinuation rate at 6 weeks and 6 months.
Methods: Retrospective, cross-sectional study conducted at the Department of Obstetrics and Gynecology, Lahore General Hospital, Pakistan, from May 2015 to August 2019. The data were collected and analysed after approval from the hospital ethical committee and were retrieved from the maternal and neonatal child health programme. Record of clinical visit and telephonic survey for miscellaneous complaints at 6 weeks and 6 months were evaluated from the medical records department and relevant data were extracted. The data were analysed using the IBM Statistical Package for the Social Sciences (SPSS® Statistics) V21.0 software (International Business Machines Corporation [IBM], New York, USA) and the results were expressed in descriptive statistics in frequencies and percentages.
Results: Total live births during the study period were 43,065. A PPIUCD was inserted in 5,275 females (12.24%). Only 13% presented for clinical follow-up; 87% had a telephonic conversation. Of these, 33% were advised to have a clinical visit and 83% reported no complaints. Reassurance was needed in 11% and threads were trimmed in 2%. Problems reported were displaced intrauterine contraceptive device (IUCD; 3.3%); spontaneous expulsion (24.0%); vaginal infections (4.7%); missing strings (3.0%); cramping (25.0%); dyspareunia (6.0%); spotting (52.0%); and vaginal discharge (16.0%). Ultrasound was advised (3.0%), as were symptomatic treatment (14.0%) and antibiotics and IUCD removal (0.7%). IUCD was discontinued by 6.7% of the females for various reasons: family pressure (0.3%); wanting a further child (0.7%); and opting for another method of family planning (14.0%). IUCD was removed and reinserted in 4.9%.
Conclusion: PPIUCD has a low turnover rate of follow-up but has high compliance with devices and a low complication rate; however, complications can be reduced by improving patient selection and clinical follow-up. It provides an excellent window of opportunity for providing effective long-term contraception to the patients who need it the most.
Key Points
1. Consecutive pregnancies spaced less than 24 months apart carry a higher risk of premature labour, miscarriage, low birth weight, post-partum haemorrhage, and foetal loss. Spacing out pregnancies by 2 years could avert 10% of child and one-third of maternal deaths.
2. This retrospective, cross-sectional study analysed data on the clinical follow up of the insertion of post-placental intrauterine contraceptive devices in 5,275 females in Lahore General Hospital, Pakistan.
3. Misconceptions around the use of intrauterine devices at community level remain an issue, however, multiple studies have indicated high continuation and satisfaction rates.
INTRODUCTION
Pakistan is referred to as sixth most populated country in the world. In 37% of females, the gap between two births is almost less than 24 months. Contraceptive use is highest in those aged between 34–36 years. Between various reversible family planning methods, couples usually use either condoms or injectable contraceptives. The female sterilisation method is used as a permanent method. Recently, family planning resources have reported 64.4% unmet needs, which is leading to low contraceptive prevalence in Pakistan.1
One-third of maternal deaths and 10% of child mortality can be averted by family planning, which happens when pregnancies are spaced by couples for more than 2 years apart.2 Small gaps between the births are linked with higher child mortality and higher maternal morbidity and mortality.3 With respect to the previous birth, pregnancies taking place within the time period of 24 months show a higher risk of premature labour, miscarriages, low birth weight babies, post-partum haemorrhage, and fetal loss. From 2005–2006, India’s National Family Health Survey (NFHS) confirmed that 61% of births were spaced less than 3 years4 and that 22% of married females had an unmet need for family planning. In India, 65% of females have an unmet need for contraceptives in the first year post-partum, for family planning.5 Post-placental intrauterine contraceptive device (PPIUCD) insertion is a convenient, safe, and effective method for post-partum contraception.6 After the removal of the placenta, immediate intrauterine device (IUD) insertion has not been associated with uterine subinvolution, increased risk of uterine perforation, post-partum bleeding, or increased infection.7 It was observed that expulsion rate was higher in immediate PPIUD insertion when compared with insertion at an interval of 4–8 weeks.
IUDs are a safe, highly effective, and long-acting form of contraception. Since the 1960s, the concept of IUD insertion as a post-partum IUD has become acceptable and has been investigated worldwide. Where females have access to medical care, IUD delivery provides a significant opportunity for the contraception need. Post-partum family planning is accepted to prevent closely spaced and unintended pregnancies in the first 12 months following childbirth.7 Effective contraceptive methods are a major need in order to prevent an unplanned pregnancy within a short interval.8
According to World Health Organization (WHO) Medical Eligibility Criteria, the insertion of an intrauterine contraceptive device (IUCD) can be done within 48 hours post-partum.9 According to the availability of options, the copper T (CuT) 380A IUD, which has a multi-year cost, is considered to be the most cost-effective contraceptive option available. The CuT 380A IUD is a non-hormonal and effective method that can be used by all females, regardless of their breastfeeding status.10 IUCD is a long-acting reversible method of contraception with 12 million current users worldwide.
METHODOLOGY
This paper outlines a retrospective, cross-sectional study conducted in the Department of Obstetrics and Gynecology, Lahore General Hospital, Pakistan, from May 2015 to August 2019. The study was conducted after approval from the hospital ethical committee. The total live births during the study period were 43,065; PPIUCD was inserted in 5,275 females (12.24%). The comparative data of patients’ clinical follow-ups, visits, and problems were assessed using the IBM Statistical Package for the Social Sciences (SPSS® Statistics) V21.0 software (International Business Machines Corporation [IBM], New York, USA), and the results were expressed in descriptive statistics in frequencies and percentages.
RESULT AND DISCUSSION
This retrospective study of PPIUCD insertion was conducted from May 2015 to August 2019 in a tertiary centre in Pakistan. PPIUCD insertions in 5,275 females showed that a large number of females agreed to space out their next pregnancy with the choice of insertion of an IUCD immediately after removal of the placenta and within 30 minutes of delivery. To signify the use of PPIUCD, counselling of the couple should occur in the antenatal period and before delivery, which can be very effective in having them leave the hospital already protected against unplanned pregnancy. After the removal of the placenta, immediate insertion of an IUD satisfies the basic requirements of contraceptive methods.11 Other females accepted this contraceptive method because they did not want any more children. The complications and issues associated with this method were also very low. To limit future childbearing, females mostly accepted the method and indicated the PPIUCD as their long-acting reversible contraceptive method.12
The majority of females (as high as 83%) reported accepting PPIUCD as a method of contraception because it is long-acting (Table 1), while many females (22%) accepted the PPIUCD insertion due to its free-of-cost service. Significantly, 50% of the females had heard of the IUCD before they were consulted at the facility, and only 7% had used one before they visited the facility, hence the vast majority of clients had accepted the PPIUCD service.13 During this study, it was also observed that nearly all females were satisfied at the time of IUCD insertion, and it was reported that they were happy with IUCD at 6 weeks following insertion of the device.
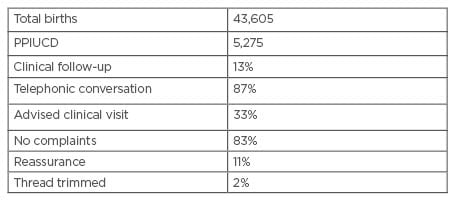
Table 1: Total births during study period.
PPIUCD: post-placental intrauterine contraceptive device.
In the present study, out of the females who discontinued the use of PPIUCD: 1% of females faced family pressure to discontinue the method; 4% wanted a future child, so discontinued the use of this method; and 70% of females opted for another method of contraception. Some users experienced side effects and others reported the removal and reinsertion of the IUCD due to other reasons (0.25%). The common issues (Figure 1) associated with this method of contraception were noted as being: displacement of IUCD (3.3%); vaginal infections (4.7%); missing strings (3.0%); cramping (25.0%); dyspareunia (6.0%); vaginal discharge (62.0%); and vaginal spotting and bleeding (52.0%). About 3.8% of females had removed their PPIUCD within the first 6 weeks of insertion. For minor issues, some of the users were advised symptomatic treatment (14.0%), some had to undergo a pelvic ultrasound (3.0%), while others had infections for which they needed antibiotics and IUCD removal (0.7% [hl]Figure 2[/hl]).
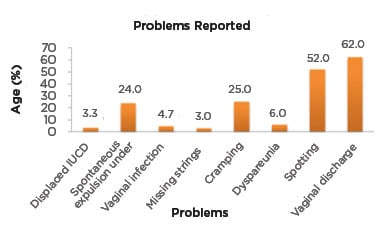
Figure 1: Data of the issues reported.
IUCD: intrauterine contraceptive device.
There is a room for strengthening PPIUCD counselling services regarding complications, such as uterine perforation and other common side effects that arise from IUCD use, which lead to the discontinuation of this suitable method of contraception.14,15 Awareness of the common issues associated with the use of the PPIUCD in the antenatal period prior to insertion would be expected to have a positive effect on the continuation of the use of this method. Counselling about minor issues and ease of treatment would be associated with a reduction or discontinuation of the PPIUCD use. Doubts of users should be addressed before its insertion, just after delivery.16
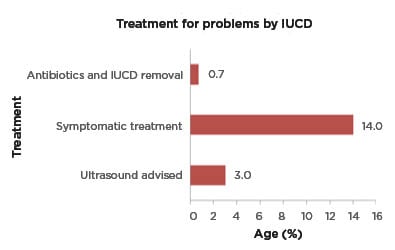
Figure 2: Treatment for issues from the intrauterine contraceptive device.
IUCD: intrauterine contraceptive device.
In the authors’ case, the continuation rate of use of PPIUCD was observed as >75 per 100 users for CuT 380 devices, showing the acceptability of post-placental insertion of IUCD as an effective and safe method of long-term contraception.
By educating the target population, the attitude towards traditional methods has changed, as have concerns about their safety due to developing innovations in family planning practices. Recent studies that were done on the post-partum contraceptives used among adolescent mothers confirmed a lower risk of rapid repeat pregnancy in those using long-acting reversible contraceptive methods than in those who adopted short methods such as oral contraceptive pills.17
A detailed study of immediate PPIUD indicated that its insertion neither increased the risk of infection nor the amount of bleeding. In various reports, CuT IUDs had a higher expulsion rate when inserted after delivery following the removal of the placenta compared with delayed insertion.18
Many females are accepting this method to limit them bearing future children, showing the important place that PPIUCDs hold as a long-acting reversible contraceptive method. In terms of policy implementation, the family planning programme has transformed to assist in fertility control and has been stressing the cafeteria approach. In the cafeteria approach, various contraceptive methods are offered to clients, where they can select their contraception based on their age, profession, parity, social class, and duration of birth spacing required.19
Effective contraception after childbirth assists in the health improvement of mothers and infants, whilst giving mothers time to bond with their babies. Rates of major maternal complications like third-trimester bleeding, anaemia, puerperal endometritis, and death all decrease due to the longer birth interval, thereby improving the quality of life of both mother and baby. In females who are breastfeeding, contraception with PPIUD is highly effective and does not impair lactation. Lactation is an essential aspect of motherhood, especially in the immediate post-partum. Multiple methods have been restricted in females who are lactating in the immediate post-partum period, hindering effective contraception; however, PPIUD insertion has no contraindications to its use during lactation and can be used freely in females who are lactating.20
To overcome the risks to infant health and maternal health outcomes, in 2005 the WHO recommended a waiting time period of 24 months after birth before attempting the next pregnancy. The acceptability of post-partum IUCD insertions can be enhanced by developing awareness in the target population of these as an effective, hassle-free method of long-term contraception.
It was observed that, for most females, the husband was the decision-maker in family planning decisions and was playing a vital role in the choice of contraceptive methods to be chosen by the couple. Despite providing proper counselling to the females during the antenatal period, most of them did not follow what they had decided before. Therefore, counselling sessions for couples are recommended for females seeking hospital deliveries in order to prevent miscommunication and avoid a change of decision for the couples. The contraceptive method selection is equally important, so decision-makers should be aligned in their choice of method once they agree on contraception after childbirth.21 In certain studies, it was noted that in some cases the mother-in-law opposed (1.4%) and, in other cases, the husband did not allow for post-partum IUCD insertion (11.0%); some clients stated another reason (2.8%), such as a decline in sexual activity following the IUD insertion.
In Mexico, family planning has been included in antenatal services and counselling is substituted into routine pre-natal care. This change has brought improvement to the contraceptive practices, and the sterilisation rate is increasing significantly with pre-natal family planning counselling. Studies from Mexico prove this change is effective in the antenatal counselling of couples.22 Although no randomised controlled trials have evaluated the expulsion rates of IUD insertion at the time of caesarean section delivery in comparison to vaginal delivery, it was found by one cohort study that there was a lower expulsion rate with IUD insertion at the time of delivery compared with insertion within 48 hours after birth.23
At a community level, misconceptions are still an issue. IUD has been associated with taboos and religious disbelief but, in multiple studies, satisfaction rates were extremely high, as well as continuation rates of post-placental IUD use.
CONCLUSION
PPIUCD has higher rates of expulsion and other minor complications compared with interval IUCD. It is a trade-off between greater contraceptive coverage versus a slightly higher complication rate; however, complications can be reduced by improving patient selection, comprehensive clinical follow-up, and early counselling. The use of PPIUCD offers an excellent window of opportunity for providing effective long-term contraception to the patients who need it most and the nations that are expected to have a population explosion.








