Abstract
Background: Cervical cancer is preventable when detected early by screening for the presence of abnormal cells on the uterine cervix. This study assessed awareness and utilisation of cervical cancer screening services among mothers attending antenatal and postnatal clinics at State Hospital, Ijebu-Ode, Nigeria.
Methods: In this descriptive cross-sectional study, the authors used a simple random sampling technique to select 330 respondents. Two hundred and twenty-one and 109 respondents from antenatal and postnatal clinics, respectively, were selected randomly. Participants were required to complete a self-structured questionnaire at both clinics, and the collected data was analysed using a statistical package for social sciences (SPSS).
Results: The mean age of the respondents was 27±1.29 years, with the majority being married. While 59.8% of the women were aware of cervical cancer screening, the utilisation of cervical cancer screening services was low, with the majority (63.9%) never having undergone the screening. Factors like young age, insufficient knowledge, and lack of awareness of cervical cancer screening services affected its utilisation.
Conclusion: Results indicate an urgent need for the promotion of healthcare-seeking behaviours by relevant stakeholders. Avenues for promoting this could be awareness programmes about the availability of screening services and their benefits, through media, places of worship, women’s groups, and during routine medical checks. This will improve cervical cancer screening utilisation services among women, thereby reducing morbidity and mortality from cervical cancer in Sub-Saharan Africa.
Key Points
1. This is a descriptive cross-sectional survey investigating awareness of cervical cancer screeningand its utilisation among mothers attending antenatal and postnatal clinics at a State Hospital in Nigeria.
2. While awareness of cervical cancer screening among mothers was high, utilisation of screening services was low.
3. Poor uptake of cervical cancer screening services among women of reproductive age will have a detrimental effect on morbidity and mortality in cervical cancer. Significant interventions are urgently needed to encourage women to seek healthcare.
INTRODUCTION
Cervical cancer begins in the epithelial cells of the cervix following an ongoing period of infection with high-risk types of human papillomavirus (HPV). Cancerous cells begin to develop and invade the cervix and surrounding tissues over time if they are not quickly eliminated.1 In 2022, there were 660,000 new cases of cervical cancer worldwide, ranking it as the 4th most frequent cancer amongst females.2 Furthermore, out of the 660,000 women who received cervical cancer diagnoses, more than half of them passed away from the disease.2
Over 90% of cervical cancer diagnoses and deaths occur in low- and middle-income countries in sub-Saharan Africa, Central America, and Southeast Asia.2,3 Furthermore, cervical cancer is the main cause of cancer-related mortality for women in low-resource nations, particularly in Africa.2 In Nigeria, cervical cancer is the 2nd most common malignancy among females aged 15–44 years.4
According to current statistics, every year 12,075 women are diagnosed with cervical cancer, and amongst them, 7,968 die as a result of the disease.4 Cervical HPV 16 or 18 infections are thought to affect 3.5% of women in the general population at any point in time.4 These infections account for 66.9% of invasive cervical cancer cases.4 Elevated cervical cancer risk is associated with increased HPV serotype 16 and 18 infection, which are implicated in 70–75% of cervical cancer cases globally.5
Additional risk factors include socioeconomic and cultural variables like gender bias, obesity, poverty, poor diet, inactivity, excessive alcohol intake, exposure to ionising radiation, environmental contaminants, and infections (such as Helicobacter pylori, hepatitis B and C, Epstein–Barr virus, and HIV).2,6 Geographic disparities in the incidence of cervical cancer are associated with unequal access to services for immunisation, screening, and treatment.2
The established efficiency of intervention measures like immunisation against the most oncogenic HPV subtypes and screening, especially with HPV-based methods, makes cervical cancer a largely preventable disease.7 If substantial action is not taken, it is predicted that by 2030, there will be approximately 700,000 cases worldwide and 400,000 mortalities from cervical cancer, a rise of 21% and 27%, respectively.5
A medical examination of the cervix and its cells is known as cervical cancer screening. Its goal is to find precancerous cervical cell changes before symptoms arise. Treatment can prevent cervical cancer from developing at this point because, by the time a person is symptomatic, the disease may have spread and become more difficult to treat.1
A study on awareness, knowledge, and screening for cervical cancer among women of a faith-based organisation in Nigeria documented that awareness of cervical cancer screening was high (68.1%) among the respondents.8 A similar study conducted among female undergraduates in Ogun State found that the majority of respondents (68.4%) were aware of the procedure.9 However, a descriptive cross-sectional study using a convenience sample technique among 289 women of childbearing age, in the same community, in Ogun State, on knowledge of cervical cancer and awareness of its screening, discovered that 39% of the women were aware of cervical cancer screening.10 Furthermore, research in Ibadan, Nigeria, revealed that cervical screening uptake was very low amongst the respondents.11 Similarly, a research from Ethiopia documented that the level of utilisation was low, with only 14.2% of participants had ever undergone the procedure.12 Another study among women in the Gwafan community, North-Central Nigeria, found that mothers’ participation in cervical cancer screening was low.13 Additionally, a study carried out among healthcare practitioners in low-resource settings found that only 20.6% of respondents had ever undergone cervical cancer screening.14 Moreover, a systematic review on cervical cancer screening uptake among women of reproductive age in Sub-Saharan Africa found that the uptake of pap smear tests was low, at 12.87%.15
There are three types of factors that may affect mothers’ uptake of cervical cancer screening: psychosocial, organisational, and demographic, such as age, income, education, marital status, beliefs, knowledge, and fear of discomfort and embarrassment.16
In a study by Abugu et al.,8 respondents gave a variety of reasons for not taking part in the cervical screening programme, including not knowing the significance of getting screened (40.9%), not feeling susceptible to cervical cancer (18.2%), and not knowing about cervical cancer screening (69.7%). Another study on obstacles to the uptake of cervical cancer screening and treatment identified poor awareness of screening services, personal factors, painful procedures, and financial constraints as individual-related barriers to screening.16 The impediments at the institutional level were misdiagnosis, perceived lack of privacy, and the attitude of health workers. The socio-cultural aspects of the respondents’ belief systems or religion, such as the conviction that infidelity is the cause of the illness or that it is a divine punishment, their belief in traditional medicine, church or spiritual healing centres for divine intervention, and influence of their husbands and in-laws in decision-making that are typically prevalent in rural communities.16 The respondents cited policy-level impediments to the uptake of cervical cancer screening as being low education/campaigns on the disease and insufficient screening facilities.16 In addition, an analysis of the variables influencing cervical cancer screening among Asian women identified obstacles to its use, such as knowledge, attitudes and beliefs, perceived risk, psychological variables, self-efficacy, past experiences, time, home, culture, fatalism, social support, access, cost, safety, insurance, and variables connected to the health system.17
Furthermore, an investigation into the factors that motivate women to undergo cervical cancer screening in Ibadan revealed personal obstacles to screening uptake, including anxiety about unfavourable test results, discomfort associated with the process, and cultural and religious constraints, including being attended to by male medical personnel.11 A small percentage of women believed they were not at risk for cervical cancer, and others were scared of being classified as promiscuous.11 Previous studies documented that improved cervical cancer screening rates among women can be achieved through care-seeking behaviour interventions, which include screening services without financial implication, female midwives collecting samples, providing printed materials, oral invitations, and encouragement by peers, women leaders, and other influential figures, as well as clients’ reminders and brochures.18-20 In a related study, a strategic trial on tactics to boost uptake among young women invited for their first cervical screening, it was found that encouraging women to get screened for cervical cancer could not be achieved by offering a nurse navigator, giving them the option of timed appointments, or by providing a self-sample kit upon request.21
RESEARCH OBJECTIVE
Cervical cancer continues to be the leading cause of cancer-related deaths among women in resource-limited settings, even though it is avoidable if detected and treated early.2,3 Without significant interventions, there is a greater possibility of an upsurge in the number of cervical cancer diagnosis and mortality globally.2,5 Therefore, significant interventions such as effective cervical cancer screening programmes for HPV infection serotypes 16 or 18, which is the causative agent among women at risk; early treatment of this infection or any abnormal cervical changes if present; as well as positive healthcare-seeking behaviour of women at risk of this infection, will drastically decrease the prevalence and burden of cervical cancer cases.2
MAIN OBJECTIVE
The study’s main objective was to assess the awareness and utilisation of cervical cancer screening services among mothers attending the antenatal and postnatal clinic at State Hospital, Ijebu-Ode, Nigeria.
Specific Objectives
- To determine the level of awareness of cervical cancer among mothers attending antenatal and postnatal clinics at State Hospital, Ijebu-Ode.
- To evaluate the level of utilisation of cervical cancer screening services among mothers attending antenatal and postnatal clinics at State Hospital, Ijebu-Ode.
- To identify factors influencing the utilisation of cervical cancer screening services among mothers attending antenatal and postnatal clinics at State Hospital, Ijebu-Ode
- To highlight ways of overcoming barriers associated with the utilisation of cervical cancer screening services among mothers attending antenatal and postnatal clinics at State Hospital, Ijebu-Ode.
METHODS
Research Area
The research was carried out at State Hospital, Ijebu-Ode, within the Ijebu-Ode Local Government Area of Ogun State. Ijebu-Ode has a population of about 154,032 and occupies an area of 192 km2.22
Study Design
A quantitative descriptive cross-sectional survey was utilised.
Population and Sampling
The target population consisted of women within the age group of 18–50 years attending prenatal and postnatal clinics at State Hospital, Ijebu-Ode. The population was taken from clinic attendance registers of both clinics comprising 1,200 women, 800 from antenatal and 400 from postnatal clinics.
The sample size was calculated using Taro Yamane’s formula which was developed in 1967 and is stated below:
n=N/1+ [N (e2)]Where n is sample size, N is number of the study population (1,200), and e is the level of precision or relative error of estimation: 0.05n=1,200/1+[1,200x(0.05)2]
n=300
An expected 10% non-response was added, which gave a final sample size of 330.
Population proportional distribution
Antenatal population size: 800/1200 x 100=67%
Postnatal population size: 400/1200 x 100=33%
Questionnaire distribution
Women attending the antenatal clinic: 67/100 x 330=221 respondents
Women attending the postnatal clinic: 33/100 x 330=109 respondents
A convenient sampling technique was used to choose the respondents.
Instrument for Data Collection
Information was obtained from respondents with a self-developed questionnaire called the Awareness and Utilization of Cervical Cancer Screening Questionnaire (AUCSQ). It has five sections: ‘A’, ‘B’, ‘C’, ‘D’, and ‘E’. Section A obtained data on the demographic characteristics of the respondents. Section B focused on the level of awareness of the women about cervical cancer screening in an adapted option ‘Yes’ or ‘No’. Section C contained items with four-point Likert scale options (4 being ‘frequently’, 3 being ‘occasionally’, 2 being ‘rarely’, and 1 being ‘I don’t do it’) to collect information on the use of cervical screening services. Section D focused on the variables influencing the use of cervical cancer screening services by mothers attending antenatal and postnatal clinics with ‘Yes’ or ‘No’ options. Section E contained items to identify ways of improving cervical screening among mothers attending antenatal and postnatal clinics. It was prepared to select either ‘Agree’ or ‘Disagree’ preferences. The tool was written in English and interpreted for illiterate respondents in Yoruba and Ijebu local dialect.
Validation of survey tool
The questionnaire was reviewed by experts in maternity nursing and oncology before its final administration to respondents.
Reliability of survey tool
The test-retest approach was used to decide how reliable the instrument was. A pilot study was conducted with twenty women who were not included in the sample. They were selected from GRA, Ijebu-Ode, Oke Oyinbo Health Centre.
Method of Data Collection
Prior to the distribution of the study questionnaire, permission for conducting the study was obtained from clinic co-ordinators by the researchers. Rapport was established with the respondents by the researchers, the objectives of the study were explained to them, and their permission was sought before any questionnaires were distributed. The respondents were given assurance of the confidentiality of their responses, as they were for research purposes only. The questionnaires were administered to 330 respondents between 10 am and 12 pm throughout the clinic days of a week by the researcher to target women in prenatal and postnatal clinics. The researchers solicited the help of the nursing staff working in the clinics for the distribution and collection of questionnaires.
Method of Data Analysis
Using the Statistical Package for Social Science (SPSS; International Business Machines Corporation, New York, USA) software version 21, data collected were coded into a computer system. Descriptive statistics of frequency, percentages, means, and standard deviations were used to analyse the research objectives.
Ethical Considerations
The research was authorised by the Babcock University Health Research and Ethics Committee (BUHREC516/18), and an administrative permit was obtained from the appropriate hospital authorities. Respondents’ informed consent was obtained after they were informed of the objectives of the study through the language they understood. The anonymity and confidentiality of respondents were ensured by transcribing all data using codes.
RESULTS
Three hundred questionnaires were administered, but 296 questionnaires (99% response rate) were retrieved for analysis.
Socio-Demographic Data of Respondents
Most of the respondents (36.5%) were found to be between the ages of 25–29 years, while the least (4.1%) were between the ages of 45–49 years. Of respondants, 76% were married, and 56.1% practice Islam as their religion. The majority (52%) were graduates of tertiary institutions, while 44.3% were self-employed. Many (44.3%) respondents commenced sexual activities at the age of 19–21 years, with an average of 20±0.86 years. Most (80.1%) had no experience of sexually transmitted infection.
Awareness of Cervical Cancer Among Mothers attending Antenatal and Postnatal Clinics
The study found that awareness of cervical cancer screening was high among respondents, as the majority (59.8%) of women attending antenatal and postnatal clinics were aware of cervical cancer screening. Most of them (64.2%) learnt about it through nurses. Furthermore, over half of the respondents (63.9%) were unsure if women under the age of 20 years could get screened for cervical cancer (Table 1).
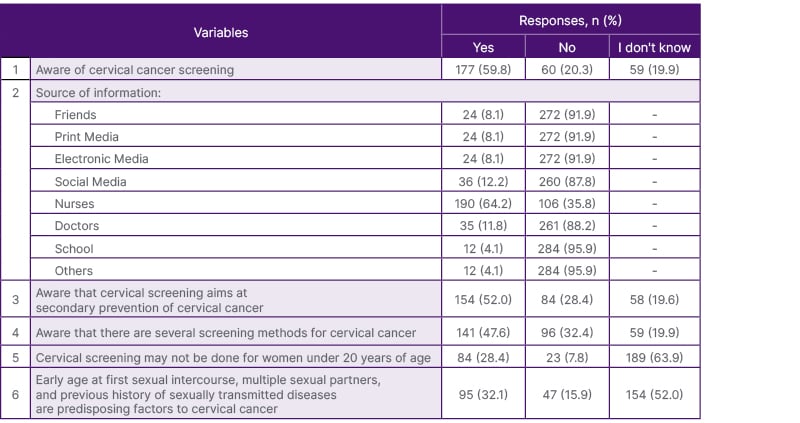
Table 1: Awareness of cervical cancer among respondents.
Utilisation of Cervical Cancer Screening Services Among Respondents
Findings depicted that a high proportion (72.6%) of respondents agreed that there is no provision for a screening centre in their area. Most (84.5%) of the respondents had not performed the screening due to screening cost. Meanwhile, out of 15.5% of respondents who had performed the screening, only 11.5% of them performed it once (Table 3). Overall, the level of use of cervical cancer testing was low amongst the women, as the majority (63.9%) of them had never undergone the screening before (Table 2).
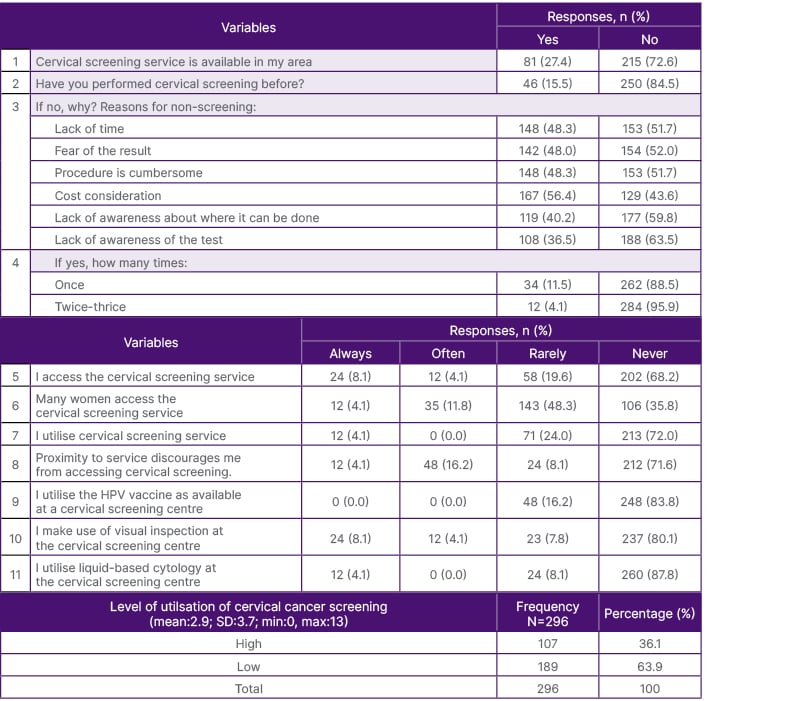
Table 2: Utilisation of cervical cancer screening services among respondents.
HPV: human papillomavirus; SD: standard deviation.
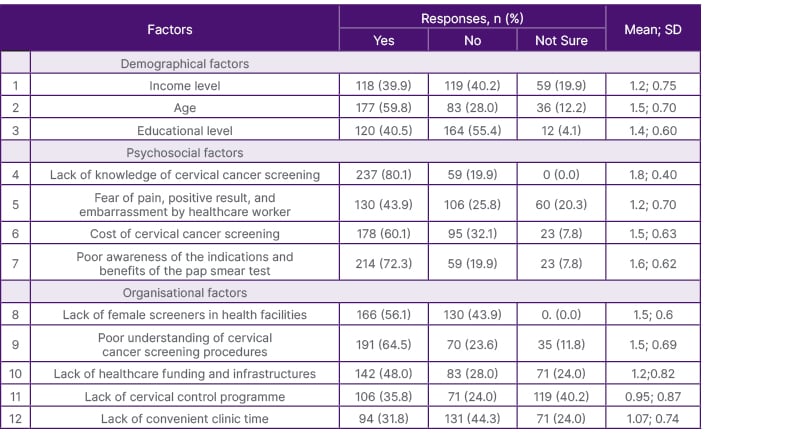
Table 3: Factors influencing utilisation of cervical cancer screening services among respondents.
SD: standard deviation.
Factors Influencing Respondents’ Use of Cervical Cancer Screening Services
According to the results of this survey, the majority, 40.2% and 55.4% of respondents claimed that income level and educational level, respectively, do not affect the use of cervical cancer screening services. However, the majority, 59.8%, 80.1%, 60.1%, and 72.3% of respondents agreed that age, inadequate understanding of the procedure, cost of the test, and ignorance of the indications and benefits of the screening, respectively, are possible reasons that could have an impact on women’s utilisation of cervical cancer testing services. Furthermore, 56.1% of the respondents were in agreement that the lack of female screeners in healthcare facilities affected the utilisation of cervical cancer assessment services. While fewer (44.3%) respondents concurred that lack of convenient clinic time will not affect the use of cervical cancer assessment services amongst women (Table 3).
Ways of Overcoming Barriers Related to Cervical Cancer Screening Services Amongst Mothers
Findings revealed that almost 95.9%, 83.8%, and 80.1% of the respondents concurred that more public awareness programmes such as sharing of posters and flyers, public enlightenment on social media, and health talks at marketplaces as done for HIV/AIDS, respectively, will be useful tools for overcoming hurdles of cervical cancer screening services amongst women. Additionally, most women (95.9%) suggested that cervical cancer screening should be made known to both educated and uneducated people. The majority (76%) also agreed that cervical cancer screening should be part of the topics discussed during antenatal clinics.
DISCUSSION
The average age of participants was 27±1.29 years. The majority were married (76%) and graduates of tertiary institutions (52%). Furthermore, 44.3% were self-employed and 35.8% were unemployed. The current research found that most women attending prenatal and postnatal clinics (59.8%) were aware of cervical cancer screening. The results are consistent with the findings of past studies, in which respondents had a high level of awareness regarding cervical cancer screening.8,9 However, the finding varies from similar studies that documented respondents’ inadequate knowledge of cervical cancer screening.10,11 This could mean that environmental factors, such as home or work locations, could have led to exposure to health-related information that improved their awareness of cervical cancer screening services. For instance, awareness of cervical cancer screening was high in a previous study conducted among women in an advanced learning environment such as a university.9 However, in similar studies carried out among women in the community, awareness was low,10 despite the alarmingly high incidence and mortality rate of cervical cancer in low- and middle-income countries.
Furthermore, the use of cervical cancer screening was low among mothers attending antenatal and postnatal clinics, as the majority (63.9%) had never undergone the screening before. This finding corroborates similar studies that documented a low percentage of cervical cancer screening use among respondents.12-15 This is concerning, as respondents’ high level of awareness of the significance of cervical cancer screening for early diagnosis, prompt treatment, and prevention of mortality does not correspond to their use of the procedure. In contrast, a meta-analysis of seven studies conducted in Sub-Saharan Africa found that knowledge about cervical cancer increased screening uptake by nearly five-fold.15 Low utilisation of screening services amongst respondents in the current study and in similar studies is likely a key factor contributing to the high cervical cancer prevalence and mortality in Sub-Saharan Africa.2,3
The author’s study found that the age of women, lack of awareness regarding cervical cancer screening, financial constraints, ignorance of the benefits of the screening, lack of female screeners in the healthcare facilities, and lack of healthcare funding, including infrastructures such as screening centres, could influence the use of cervical cancer screening services by mothers who visit prenatal and postnatal clinics at State Hospital, Ijebu-Ode. This result aligns with the conclusions of related research.8,11,16,17 However, in a qualitative study conducted in the Ecuadorian Province of Azuay, women and healthcare professionals, perceived different barriers to cervical cancer screening. Healthcare professionals believed that the main barriers were at the policy level (no structured screening plan; no health promotion) and at the individual level (no risk perception; personal beliefs). On the other hand, the women primarily noted organisational-level obstacles, such as lengthy wait times, restricted access to health facilities, and poor communication between patients and doctors.18
Results from participants in the current study suggested that additional public awareness campaigns should be intensified in locations where women congregate, such as in prenatal clinics, postnatal clinics, and marketplaces, as well as social media, in order to address the issue of awareness of cervical cancer screening. This finding is corroborated in similar studies, which also documented that improved healthcare-seeking behaviour interventions, such as screening services without financial implication, female midwives collecting samples, providing printed materials, oral invitations, clients’ reminders, individualised self-sample kit upon request, the option of timed appointments, and support from peers and women leaders, among others, are capable of promoting participation of women in cervical cancer screening services.19-22 Furthermore, research has shown that political will is also required to enhance cervical cancer preventive initiatives.15
LIMITATIONS OF STUDY
Problem with Data Collection from Respondents
The method of gathering data from respondents involves questionnaires; nevertheless, some respondents did not provide the requested information when completing the surveys.
Problem of Generalisation of Results
Given the study was only conducted across two health clinics, the findings might not be generalisable beyond these two clinics.
CONCLUSION
According to the findings of this study, mothers who attended antenatal and postnatal clinics at State Hospital, Ijebu-Ode, were highly aware of the screening services available for cervical cancer, but they did not make use of available resources. Significant interventions, such as education campaigns and free screenings, are urgently needed by the right parties to encourage women to seek healthcare. This would increase the number of women using cervical cancer services, reducing morbidity and mortality from cervical cancer in Sub-Saharan Africa.







