Abstract
Background: Hypertensive disorders of pregnancy remain among the most significant causes of pregnancy-related complications. The research by the Dietary Approaches to Stop Hypertension (DASH) group revealed that non-pharmacological measures and intervention such as diet can be used to control blood pressure.
Objective: This study was completed to determine the frequency of consumption of local food among females who were pregnant and their relationship with pregnancy-related hypertensive disorders.
Methods: This was a descriptive research study of females who were pregnant with pre-eclampsia (PE) and gestational hypertension (GH) who presented at the Federal Medical Centre (FMC), Abeokuta, Nigeria. During the study period (September–October 2019) at the tertiary healthcare centre, 45 subjects who were pregnant were select from a PE and GH group, and matched with 45 patients with normotension. Comparison of bean meal onsumption (gbegiri) and bone meal (gbure-oloboro) consumption in subjects who were pregnant did not reveal statistically significant differences in those with PE and GH.
Results: The findings reveal a statistically significant difference in milk consumption between females who were pregnant with mild and severe PE (p=0.019). There was also a statistically significant difference in subjects with mild and severe GH who consumed milk (p=0.003).
Key Points
1. One of the most significant causes of pregnancy-related complications is hypertensive disorders which include pre-eclampsia, gestational hypertension, chronic hypertension, and many more.
2. This comparative study examined the frequency of consumption of local food among females who were pregnant and their relationship with pregnancy-related hypertensive disorders.
3. Dietary approaches, including increasing milk consumption in females, may lower the risk of pre-eclampsia and gestational hypertension.
INTRODUCTION
The American Congress of Obstetricians and Gynecologists (ACOG) Task Force on the classification of hypertension include pre-eclampsia (PE), gestational hypertension (GH), chronic hypertension, chronic hypertension with superimposed PE, and eclampsia. GH is diagnosed from 20 weeks into gestation with the absence of proteinuria, while PE presents as newly sustained hypertension with proteinuria.1
The research by the Dietary Approaches to Stop Hypertension (DASH) group revealed that non-pharmacological measures and intervention such as diet can be used to control blood pressure.2
Diets including calcium from different local foods such as dairy products, tofu, beans, and vegetables such cabbage leaves may help to regulate blood pressure (BP). The local sources of calcium within the authors’ metropolis is mainly from a local delicacy, which majority of the population consume. The local diets that supply calcium are mainly from gbure-oloboro, also known as bone meal, and gbegiri, also known as bean meal. In addition to the local diets, females who are pregnant also consume milk and other dairy products.3,4
Calcium performs a role in normal metabolic function of the body, especially in the transmission of neural impulses, muscle contractions, and the release of hormones. In PE, tissues such as the arterial muscles and neurons function via pathways that affect BP regulation. The binding of calcium ions to activator proteins such as troponin C starts steps involved in the excitation–contraction, which leads to muscle contraction.5 The muscle protein calmodulin activates enzymes that break down muscle glycogen to provide energy for muscle contraction. At the end of excitation–contraction, calcium is exchanged outside the cell or into the endoplasmic reticulum until the next event cycle.
The mechanism where low serum calcium causes new-onset hypertension in pregnancy has been attributed to an increase in peripheral resistance and a rise in BP. This occurs due to the stimulation and release of the parathyroid hormone (PTH) and parathyroid hypertensive factor.5,6 This leads to the production of calcitriol and subsequent activation of renin angiotensin aldosterone system. Within the arterial vascular smooth muscle cells, an increase in intracellular calcium ions via signalling pathways results in vasoconstriction, an increase in peripheral resistance, and upward trends in BP.7-9
According to the MESA cohort study,10 where 3,002 males and females (59.0±9.7 years) without cardiovascular antecedents were followed up for 9 years, where a correlation was found between higher PTH serum concentrations and a higher risk of hypertension, even after adjusting for potential confounders (hazard ratio [HR]: 1.27; 95% confidence interval [CI]: 1.01–1.59)10. Furthermore, a positive relationship between serum PTH and systolic BP found that the highest quartile of serum PTH was an independent predictor of coronary heart disease in both sexes.
Lewanczuk et al.11 studied the effect of parathyroid hypertensive factor by infusing plasma from rats with hypertension and humans with hypertension into the blood of rats with normotension and found an increase in the mean arterial blood pressure of the rats. They further studied the parathyroid origin of this factor by transplanting parathyroid glands of rats with hypertension into parathyroidectomised rats with normotension. A subsequent elevation in BP was shown in the rats after transplantation.
Hypertension in pregnancy is a major cause of maternal mortality and pre-term births, with an attendant consequence of increased perinatal mortality. There are no previous documented studies in this local population on the relationship of milk consumption and other local diets among females who are pregnant with PE and GH. Most studies on milk consumption in pregnancy have not included GH and were mainly done on PE.
In addressing the identified gaps in knowledge and adding to the few existing studies on the relationship of local diets and milk consumption with PE and GH, this study aimed to determine the relationship of consumption of milk and other local food products with PE and GH among females who were pregnant in the authors’ local area.
METHODS
The study was carried out at the tertiary healthcare centre, Federal Medical Centre (FMC), Abeokuta, Nigeria, which is one of the public hospitals handling referrals from lower treatment centres. FMC Abeokuta offers high-level tertiary management of obstetrical and gynaecological cases, supperted by other multidisciplinary, specialist teams.
The maternity section of FMC Abeokuta used in this study includes an antenatal clinic and ward, gynaecological ward, and labour ward from the Department of Obstetrics and Gynaecology.
Abeokuta is the capital of Ogun state and is situated in the tropical region of Africa. It is situated 74 km north of Lagos along the Ogun River. Abeokuta has a population of about 593,140 people, according to the 2006 census.12
The tertiary healthcare facility used in this study is a parastatal under the Federal Ministry of Health. It is a 300-bed specialist centre that was established in 1993 and is in the Idi-Aba area, within the Abeokuta South local government area in the outskirts of the city. It has an annual average delivery rate of 1,300 live births. Ethical approval was obtained from the hospital ethics and research unit.
All females who were pregnant and with a pregnancy-related hypertensive disorder at the gestational age of 20 weeks and satisfied the criteria for diagnosis of pregnancy-induced hypertension were recruited into the study. Their BP was measured with accuracy, and their urine was checked for presence of proteinuria. Brachial systolic and diastolic BPs were measured using the sphygmomanometric auscultatory method, where the arm is level and the subject sitting down, relaxing at least 5 minutes prior to the measurement. Systolic BP was recorded as the appearance of the Korotkoff sounds (Phase I), while diastolic BP was recorded as the disappearance of the Korotkoff sounds (Phase V). BP was measured using a standardised aneroid sphygmomanometer, made by Accoson (Irvine, UK).
The eligible subjects were assigned into the three groups: PE, GH, and a third group of individuals with normal BP. One in three females who were pregnant with normal BP were selected until the required number of was achieved, while females with PE or GH who consented to the study were consecutively recruited until the required number was achieved. The subjects were matched for age, parity, socioeconomic status, and BMI. The sample size was determined by applying the formula for comparison of two mean: n=2 (u+v)2 σ2/(d)2.
A self-explanatory questionnaire was given to the subjects by the research team to collect necessary data required for the study. The questionnaire was pre-tested in the local population prior to the actual study.
The assessment of serum calcium level was determined using the o-cresolphtalein complexone technique at 570 nm absorbance.13 The normal range of serum calcium used in this study was 2.1–2.8 mmol/L. The data generated from the study was analysed with the use of IBM SPSS 23 (IBM, New York City, New York, USA).
RESULTS
An equal number of subjects (45 in each group) with the PE, GH, and normal blood pressure participated in the study. Females who were pregnant who were at the gestational age of 20 weeks or more were selected for the study.
This study found that the mean serum calcium level in subjects who consumed milk (mean±standard deviation) was 2.44±1.27, bone meal 2.55±1.32, and bean meal 2.30±0.76. This study found no association in the mean serum calcium level between the different dietary intakes (Figure 1)
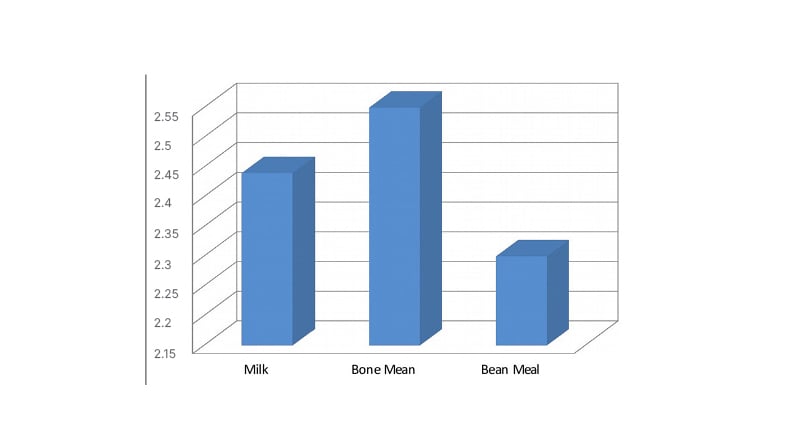
Figure 1: Dietary intake and mean serum calcium level.
The milk consumption between females who were pregnant with mild and severe PE was statistically significant (p=0.019). Females with mild GH were significantly more likely than those with severe GH to have consumed milk at least twice a day (p=0.003). Comparison of bean meal consumption (gbegiri) and bone meal (gbure-oloboro) in subjects who were pregnant did not reveal any statistically significant difference in those with PE and GH (Table 1).
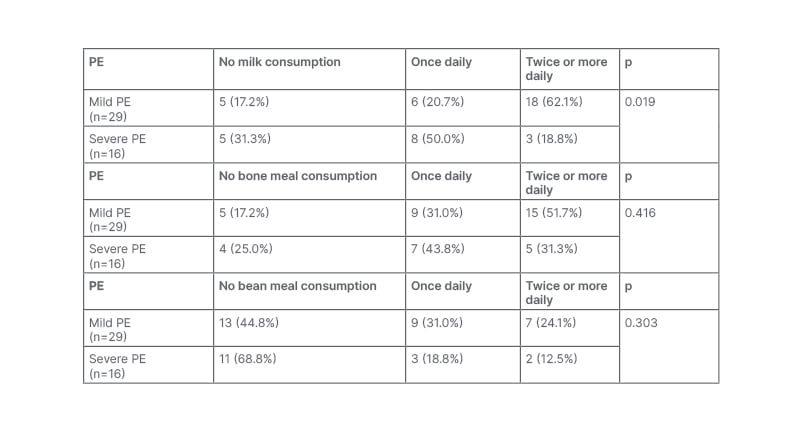
Table 1: Dietary consumption among subjects with pre-eclampsia.
There were statistically significant differences between milk consumption in subjects with mild and severe PE (p<0.05).
There were no statistically significant differences between bone consumption in subjects with mild and severe PE.
There were no statistically significant differencse between bean meal consumption in subjects with mild and severe PE.
PE: pre-eclampsia.
DISCUSSION
The findings from this study revealed that milk consumption was statistically significant (p=0.019) in females who were pregnant with mild and severe PE. This is similar to the study in Norway by Nordqvist et al.,4 which found that the intake of milk in the later weeks of pregnancy lowered the risk of PE. In the same study, milk intake was found to reduce the risk of pre-term delivery when instituted in the early part of pregnancy.4 However, this study recruited 70,149 singleton females who were pregnant,4 which is more than the number of subjects who participated in the authors’ study.
In this study, it was surprising to find that this is no direct association between serum calcium level among subjects who were normotensive and subjects with PE or GH who consumed milk with local diets. The first report on the association between PE and calcium intake was in the 1980s.5
The Mayan population who live within Guatemala were found to have low incidence of PE. This reportedly followed their unique lifestyle where they soak corn in lime, which was considered to have high content of calcium and, therefore, have a high calcium intake.5
The Ethiopian population have a similar diet high in calcium and, with a high intake of calcium, were reported to have among the lowest incidence of hypertensive disorders of pregnancy.5
Several studies have opined a possible association between PE and calcium. However, the relationship between rich dietary sources of calcium and the possible link with low prevalence of PE and GH is still a subject of controversy, probably due to the inability of studies to prove a causal link and the different mechanism of reduction of PE and GH.
Findings from the authors’ study could not prove any significant different in the level of serum calcium between participants who consumed milk and those who mainly consumed local dietary products (bean meal and bone meal). However, this study did find a statistically significant difference (p=0.003) in dietary milk consumption between participants who consumed milk with mild and severe GH.
Egeland et al.,14 a study from Norway, found that diets that are low in calcium can lead to occurrence of new-onset PE and GH among females who were childbearing with GH in previous pregnancy. According to Egeland et al.,14 adequately planned interventions that are used to increase the baseline body stores of calcium and other essential minerals can help in reducing of the burden of hypertension in pregnancy within the childbearing population.
Brantsaeta AL et al.,15 in a study of occurrence of PE in primigravida, found that consumption of milk-rich food had an inverse relationship, with incidence of PE. This may have been due to milk being rich in lactobacilli.15
From this study, local dietary meals considered to be rich source of calcium (bone meal and bean meal) in the Western part of Nigeria revealed no statistically significant differences among participants with pregnancy-related hypertensive disorders. The mechanism associated with the reduction of incidence of pregnancy-related hypertensive disorders may be due to alteration in the inflammatory process, which may also involve microbiological flora that could occur in females who consume milk.
In a cross-sectional study of the Chinese population, Chen X et al.16 found that diets consisting mainly of snacks is associated with pregnancy-related hypertensive disorders. In the Chen X et al.16 study, diets that have a lot of salt increases the risk of PE and GH.
According to a study by Hillesund et al.,17 a high New Nordic Det led to reduced overall incidence of PE and pre-term births.
Among other studies, Villegas R et al.18 found that there is reduced incidence of Type 2 diabetes in those who consume a diet rich in diary milk. Villegas R et al.18 also revealed that healthy eating habits could, by health education, lead to lower risk of endocrine and cardiovascular diseases. The close occurrence of diabetes together with hypertension remains undisputed.
Guidelines by the ACOG1 indicate that calcium can lower the risk of PE in populations that have a deficiency of calcium; however, the use of low-dose aspirin (60–80 mg) can reduce PE and adverse perinatal outcomes.1,19-21
CONCLUSION
There is possibility that milk consumption may be associated with a reduction in PE. Dietary approaches, especially increasing the milk consumption in females, may lower the risk of PE and GH.
RECOMMENDATION
Females who intend to become pregnant could benefit from advice on the need to consume milk products, which can reduce the risk and complications associated with PE and GH.







