The practice of follicle flushing has been a topic of discussion since ultrasound-guided transvaginal oocyte retrieval was introduced in 1981.1 Theoretically, flushing would allow for the retrieval of more oocytes and consequently result in greater fertilisation and pregnancy rates. However, many studies have found no significant increase in fertilisation following the use of flushing.2,3 The National Institute for Health and Care Excellence (NICE) guidelines4 suggest that follicle flushing for women with three follicles prior to oocyte retrieval should not be offered, as it increases the length of the process and the pain experienced without the added benefit of greater numbers of oocytes retrieved or higher pregnancy rates.
Data from 221 women who underwent oocyte retrieval at the University Hospital of Wales, Cardiff, UK between May 2016 and April 2017 were retrospectively evaluated. In total, 162 women were included in this study; 59 had to be excluded due to inadequate information available. Thirty-nine women (24.1%) were noted to have undergone oocyte retrieval with direct aspiration only, while the remaining 123 (75.9%) had undergone oocyte retrieval with follicle flushing.
Procedures at the centre were performed using 16-gauge double lumen needles. The flushing medium used was from Origio Ltd., Reigate, UK. Chi-square tests performed with p<0.05 were considered statistically significant. To determine a cut-off value for the number of follicles needed to be present at the point of human chorionic gonadotropin administration, a receiver operating characteristic curve was plotted and the area under the curve was calculated. SPSS statistical software (version 24), IBM, Armonk, New York, USA, was used.
The total number of oocytes (13.6±6.5 versus 7.7±5.2), the number of mature oocytes (11.7±6.4 versus 6.3±4.6), the number of fertilised oocytes (7.5±5.3 versus 4.4±3.6), the duration of procedure (21.8±7.3 minutes versus 20.2±5.6 minutes), as well as maturation (84.7% versus 83.7%) and clinical pregnancy rates (30.8% versus 22.8%) were found to be higher in the direct aspiration only group compared to the flushing group. The chi-square test indicated that all of the above, except the duration of procedure and clinical pregnancy rate, were statistically significant. On the contrary, the flushing group demonstrated higher fertilisation rates (57.8% versus 54.7%) when compared to the direct aspiration only group. However, these rates were not statistically significant. Figure 1 shows the area under the curve was measured to be 0.080 with 95% confidence interval (lower bound: 0.000; upper bound: 0.181). This area, being <0.5, implies that the cut-off value of approximately nine follicles at the point of human chorionic gonadotropin administration, below which follicle flushing would be recommended to obtain at least three mature oocytes, may not be accurate.
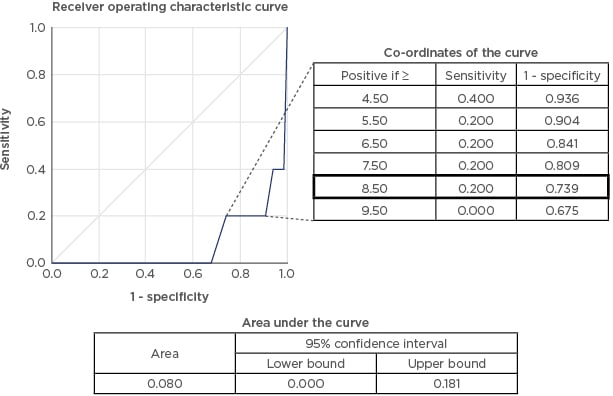
Figure 1: Receiver operating characteristic curve with the suggested cut-off point of 8.50 follicles and corresponding co-ordinates highlighted. Also shown is the area under the curve.
The suggested cut-off value of roughly nine follicles at the point of human chorionic gonadotropin administration, below which follicle flushing would be recommended to obtain at least three mature oocytes, derived from the receiver operating characteristic curve, may not be accurate due to a small area under the curve of 0.080 and the lower number of oocytes, mature oocytes, and fertilised oocytes in the flushing, compared to the direct aspiration group. Fertilisation and clinical pregnancy rates were not different between the two groups.
These findings, coupled with the first principles of surgery, which dictate that shorter and simpler procedures with minimal tissue handling can result in fewer complications, form the basis of our recommendation that follicle flushing should not be routinely performed during oocyte retrieval.








