BACKGROUND AND AIMS
Intrauterine adhesions (IUAs) are considered one of the main reproductive system diseases affecting females worldwide, characterised by endometrial fibrosis with partial to complete obliteration of the uterine cavity and/or cervical canal.1-4 The Prevention of Adhesions Post Abortion (PAPA) study showed that application of auto-crosslinked hyaluronic acid (ACP) gel, an absorbable barrier in those undergoing recurrent dilatation and curettage (D&C) for miscarriage, resulted in a lower rate of IUAs, 13% versus 31% (relative risk: 0.43; 95% confidence interval [CI]: 0.22–0.83), lower mean adhesion score and significant less moderate to severe IUAs.5 After a follow-up, the question remains if the long-term reproductive outcomes following recurrent D&C for miscarriage in individuals with identified and treated IUAs are comparable to individuals without IUAs.6
METHODS AND MATERIALS
This was a follow-up of the PAPA study, a multicentre randomised controlled trial evaluating the application of ACP gel in females undergoing recurrent D&C for miscarriage.5 In the trial, 152 females who had undergone a first-trimester miscarriage with at least one previous D&C were randomised for D&C alone or D&C with immediate intrauterine application of ACP gel. All included females who had received a diagnostic hysteroscopy 8–12 weeks after randomisation to evaluate the uterine cavity and for adhesiolysis if IUAs were present. Participants were approached at least 30 months after randomisation to evaluate reproductive performance, obstetric, and neonatal outcomes. The main outcome was ongoing pregnancy. Outcomes of subsequent pregnancies, time to conception, and time to live birth were also recorded.
RESULTS
Reproductive outcomes of individuals with and without an IUA diagnosis after a mean follow-up of 46 months are presented in Table 1. In those pursuing a pregnancy, 14/24 (58%) ongoing pregnancies were recorded in individuals with identified and treated IUAs versus 80/89 (90%) ongoing pregnancies in people without IUAs diagnosis (odds ratio [OR]: 0.18; 95% CI: 0.06–0.50, p<0.001).6 Documented live birth was also lower in those diagnosed with IUAs; 13/24 (54%) with versus 75/89 (84%) without IUAs diagnosis (OR: 0.22; 95% CI: 0.08–0.59; p=0.004). The median time to conception was 7 months in females with identified and treated IUAs versus 5 months in females without IUAs diagnosis (hazard ratio: 0.84; 95% CI: 0.54–1.33) and time to conception leading to a live birth 15 months versus 5 months (hazard ratio: 0.54; 95% CI: 0.30–0.97). In females with identified and treated IUAs, premature deliveries were recorded in 3/16 (19%) versus 4/88 (5%) in females without IUAs; p=0.01. Complications were recorded in respectively 12/16 (75%) versus 26/88 (30%); p=0.001.6 No differences were recorded in mean birth weight between the groups.
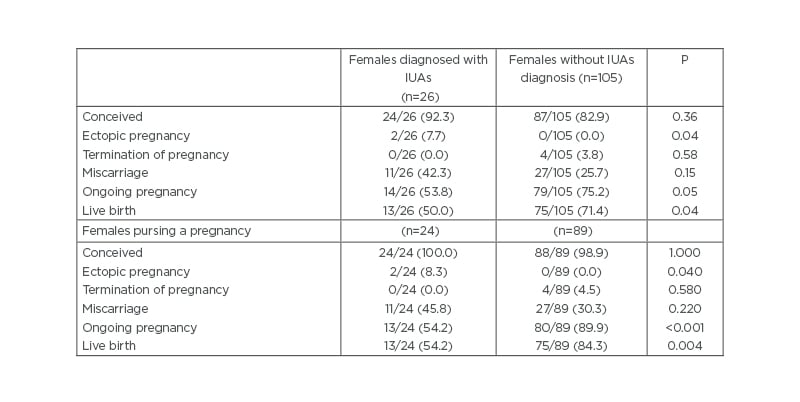
Table 1: Reproductive outcomes of females with and without intrauterine adhesions diagnosis.
IUAs: intrauterine adhesion
CONCLUSION
Reproductive outcomes in females with identified and treated IUAs following recurrent D&C for miscarriage are decreased compared to females without IUAs diagnosis. As IUAs have an impact on reproductive performance, even after hysteroscopic adhesiolysis, primary prevention is essential.
Expectative and medical management should therefore be considered as serious alternatives for D&C in females with a miscarriage. In case D&C is necessary, application of ACP gel should be considered.
LIMITATIONS AND REASONS FOR CAUTION
In the original PAPA study, randomisation was applied for ACP gel application. Comparing females with and without IUAs diagnosis is not in line with the randomisation and therefore confounding of the results cannot be excluded. IUAs, if visible during routine hysteroscopy after randomisation were removed as part of the study protocol.








