One of the most frequent causes of male infertility is failure in sperm-zona recognition and adhesion, but that cannot be diagnosed by the routine semen analysis. Many tests have been developed to assess sperm functional abilities towards the zona.1-3 It has been proven that these zona-binding tests are an effective method for predicting the fertilisation capacity of the spermatozoa and the outcomes of assisted reproductive technology.4 However, the existing methods have some practical shortcomings, such as using different zona pellucida in each test, difficulties in sperm counting, and the necessity of a healthy donor.4,5 The present study aimed to assess the predictive power of an optimised zona-adhesion assay and sperm zona-adhesion score (SZAS) on the implantation outcome.
Data on spermatozoa zona-adhesion ability and implantation success of 42 couples with male infertility factor and good quality oocytes were collected. Semen samples for standard intracytoplasmic sperm injection procedure were analysed for routine parameters according to the World Health Organization (WHO) 2010 guidelines and the SZAS was assessed. A zona-adhesion test was performed using donors’ zonae pellucidae that were acid solubilised and coated on polystyrene plates. SZAS was evaluated in samples of 250,000 motile spermatozoa by calculating the number of adhered spermatozoa per mm2 of zona-coated surface. Implantation was determined by peripheral blood human chorionic gonadotropin concentration on Day 14 after embryo transfer. Pearson correlation and t-test were used to analyse the results. Logistic regression with receiver operating characteristic (ROC) curve analysis were performed to evaluate SZAS as a predictor for the implantation outcome.
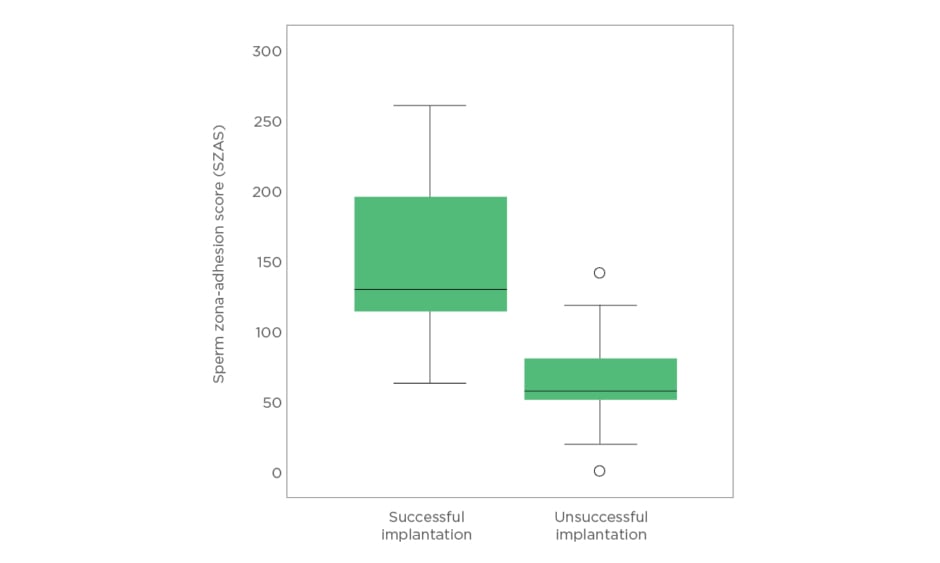
No statistical difference was observed in the common semen parameters (sperm count, concentration, motility, and morphology) between the successful (n=21) and unsuccessful (n=21) implantation groups. The evaluated SZAS did not correlate to the sperm concentration (p>0.05), sperm count (p>0.05), motility (p>0.05), or morphology (p>0.05) among the studied patients. However, as shown in Figure 1, the mean SZAS in the successful implantation group was found to be significantly higher (149±67) compared to the unsuccessful implantation group (84±37 [p=0.002]). By ROC curve analysis, SZAS predicted successful implantation with an area under the curve of 80.2% (95% confidence interval: 0.66–0.94). A cut off value for successful implantation was estimated at 65 with sensitivity 95.2% and specificity 52.4%. Moreover, logistic regression analysis identified SZAS as a significant parameter for the prediction of implantation outcome with 73.8% accuracy: 76.2% specificity and 71.7% sensitivity of the developed predictive model.
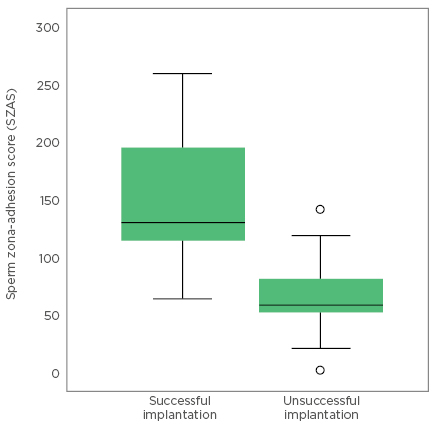
Figure 1: Sperm zona-adhesion score in the successful and the unsuccessful implantation groups.
This study demonstrates the high predictive value of the sperm zona-adhesion ability for successful implantation after intracytoplasmic sperm injection. The evaluation of SZAS could be a useful tool in directing couples with male infertility to appropriate assisted reproduction therapy.