BACKGROUND AND AIMS
Currently, there is significant evidence of an increased prevalence of maternal pregnancy complications in women with polycystic ovary syndrome (PCOS).1-4 However, there remain significant gaps in the understanding of how PCOS affects the development of gestational diabetes (GDM), gestational hypertension (GHTN), and pre-eclampsia (PEC).5,6 This is most likely because of the complex, multifactorial aetiology of PCOS, its range of potential confounders for pregnancy complications, and the variable methodology of studies that have been conducted.
To date, the largest meta-analysis on this subject includes 11,565 women with PCOS analysed for their risk of GDM and 5,896 patients analysed for their risk of PEC.2 Unfortunately, the study was unable to isolate PCOS as an independent risk factor for PEC and other hypertensive disorders of pregnancy.
The objective of this study, therefore, was to determine if PCOS confers an independent risk for the development of GDM, GHTN, and PEC, utilising the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) database. The HCUP-NIS is the largest inpatient sample database in the USA and is comprised of hospital inpatient stays submitted by hospitals throughout the country. Each year, the database provides information relating to 47 million inpatient stays, including patient characteristics, diagnosis, and procedures. The data are representative of approximately 20% of admissions to USA hospitals and represents >96% of the American population.7
MATERIALS AND METHODS
This was a retrospective, population-based cohort study utilising data from the HCUP-NIS database over 11 years from 2004 to 2014. A cohort of all deliveries between 2004 and 2014, inclusive, was created. Within this group, all deliveries to women with PCOS were identified as part of the study group (n=14,882), and the remaining deliveries were categorised as non-PCOS births and comprised the reference group (n=9,081,906). The primary outcome of this study was the prevalence of GDM, GHTN, and PEC in pregnancies of women with PCOS compared to those without PCOS.
RESULTS
At baseline, more pregnant women with PCOS were obese (22.3% versus 3.5%; p<0.001), had chronic hypertension (8.4% versus 1.8%; p<0.001), had pregestational diabetes (4.1% versus 0.9%; p<0.001), and had treated thyroid disease (12.6% versus 2.4%; p<0.001). Women with PCOS were also more likely to have undergone in vitrofertilisation (IVF) treatment (2.4% versus 0.1%; p<0.001), have multigestation pregnancies (5.9% versus 1.5%; p<0.001), and more multiple gestations in the PCOS cohort were the result of IVF treatment than the non-PCOS cohort (12.3% versus 2.3%; p<0.001).
In all pregnancies, women with PCOS were more likely to develop GDM (adjusted odds ratio [aOR]: 2.19; 95% confidence interval [CI]: 2.02–2.37), pregnancy-associated hypertension (aOR: 1.38; 95% CI: 1.27–1.50; p<0.001), GHTN (aOR: 1.47; 95% CI: 1.31–1.64), PEC (aOR: 1.29; 95% CI: 1.14–1.45), and superimposed PEC (aOR: 1.29; 95% CI: 1.04–1.59) after controlling for confounding effects (age, race, income level, insurance type, obesity, IVF use, previous caesarean section, chronic hypertension, pregestational diabetes, thyroid disease, multiple gestation, smoking, and recreational drug use). Odds ratios were comparable between all pregnancies and singleton pregnancies only. In women pregnant with multiple fetuses, PCOS only conferred a statistically significant increased risk of developing GDM (aOR: 2.33; 95% CI: 1.92–2.83; p<0.001). However, there was a trend towards an increased risk for developing pregnancy-associated hypertension (aOR: 1.92; 95% CI: 0.99–1.42; p=0.058) (Table 1).
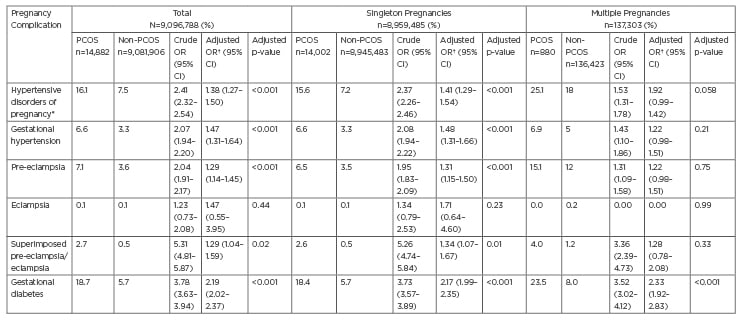
Table 1: Pregnancy outcomes of pregnant women with and without polycystic ovary syndrome, stratified by single and multiple gestations.
*Previously referred to as pregnancy-associated hypertension.
†Adjusted for age, race, income quartile, insurance plan type, hospital type, obesity, smoking, use of in vitrofertilisation, previous caesarean section, chronic hypertension, pregestational diabetes, pre-existing thyroid disease, and maternal drug use.
CI: confidence interval; OR: odds ratio; PCOS: polycystic ovary syndrome.
CONCLUSION
After controlling for all potential confounding effects, women with PCOS are at a two-fold higher risk of developing GDM, a 50% increased risk for the development of GHTN, and a 30% increased risk of developing PEC than women without PCOS. When caring for pregnant women with PCOS, it is important to also consider the risk of all other coexisting metabolic conditions frequently encountered in women with PCOS, as these risks are additive and place women with PCOS at significantly increased risk for adverse complications in pregnancy.








