Abstract
Rabies is one of the oldest communicable viral diseases affecting the nervous system of humans, caused by a rhabdovirus. It is almost always fatal, with a handful of reported survival cases. The rapid and aggressive nature of this disease poses a diagnostic challenge. Although, classical clinical history may guide the diagnosis, confirmation is obtained through microbiological tests. Radiological imaging with MRI can prove to be useful not only in the early detection of rabies but also in distinguishing it from other viral encephalitis. The authors present the clinico-radiological features of rabies encephalitis in a 3.5-year-old girl who was bitten on the left side of her face by a dog.
Key Points
1. Rabies is a rare but fatal viral disease affecting the nervous system, with a rapid and aggressive course that makes early diagnosis challenging. Imaging findings are underreported due to its swift progression.
2. This case report describes the MRI findings of rabies encephalitis in a 3.5-year-old girl following a dog bite, adding to the limited literature on imaging in rabies cases.
3. MRI can aid in the early detection of rabies encephalitis, particularly in atypical cases, helping distinguish it from other viral encephalitis and guiding public health measures to prevent further transmission.
INTRODUCTION
Rabies is one of the oldest communicable diseases known to humans and is almost always fatal, with very few cases of survival reported.1,2 It is a viral illness that primarily affects the nervous system, caused by a rhabdovirus. The rapid and aggressive nature of the disease makes it challenging to diagnose using imaging techniques. While the definitive diagnosis is made through microbiological tests, such as isolating the virus or detecting its antigens/antibodies, the diagnosis is typically based on clinical presentation and supported by radiological imaging, particularly MRI. MRI can be useful in the early detection of rabies and also in distinguishing it from other forms of viral encephalitis.
The novelty of this paper lies in the fact that rabies encephalitis is so fatal and aggressive that there is usually no time available for imaging, and thus it is not performed in the majority of clinically suspected cases. Owing to this reason, limited reports are available in the radiology literature describing the MRI brain findings of rabies encephalitis. The authors contribute to the previously existing paucity of literature by adding one case of fatal rabies encephalitis, depicting the detailed MRI imaging features in a dog-bitten child (Figure 1 and 2). Having knowledge about the imaging features would help in dispensing the early appropriate diagnosis, thereby guiding clinicians towards adequate management.
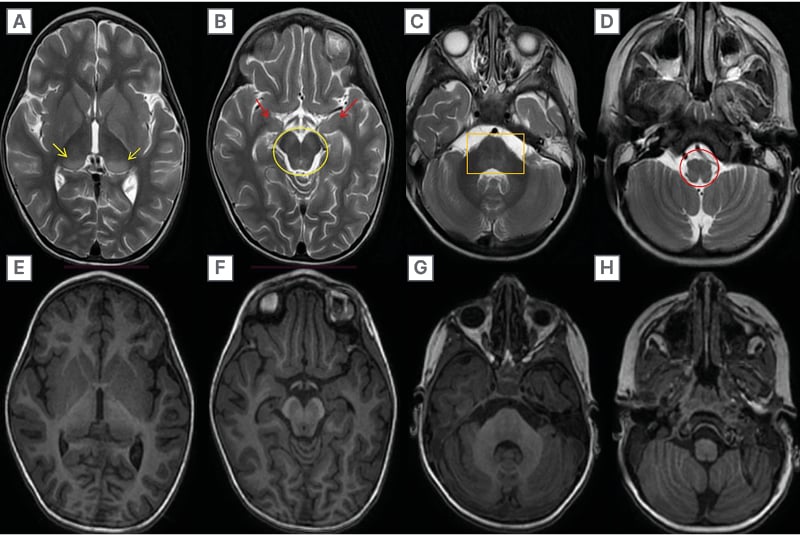
Figure 1: T2-weighted MRI Brain axial sections.
T2-weighted MRI Brain axial sections show A) hyperintensity involving bilateral basal ganglia, posterior thalami (yellow arrows), B) bilateral substantia nigra & peri-aqueductal grey matter (yellow circle), bilateral hippocampi (red arrows), C) pontine tegmentum (orange rectangle), D) and dorsal part of medulla (red circle). E–H) Corresponding T1-weighted axial sections show hypointense signal in these areas.
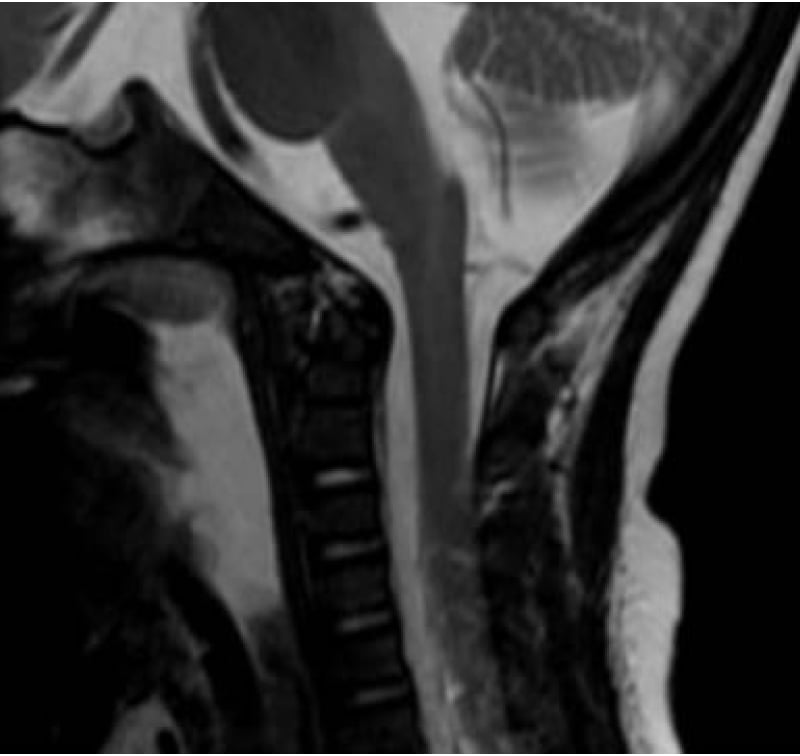
Figure 2: T2-weighted brain and cervical spine MRI sagittal section.
T2-weighted brain and cervical spine MRI sagittal section show linear hyperintense signal intensity extending from brainstem to involve upper cervical spinal cord.
CASE REPORT
A 3.5-year-old girl was bitten on the left side of the face by a dog. She received partial immunisation in the form of three doses of the anti-rabies vaccine and had rabies immunoglobulin locally infiltrated. Fourteen days after the bite, she showed prodromal symptoms, starting with a sudden onset fever and feeling unwell. It was followed by weakness in both her legs that worsened to complete paralysis over a period of 3 days. She also developed left-sided ptosis. Later, she experienced confusion and began talking to herself.
On physical examination, the girl had several lacerations on the left side of her face near her eye. Her vital signs were stable with normal fundus examination. She exhibited decreased muscle tone in all four limbs with areflexia. There were no signs of meningitis. Cerebrospinal fluid analysis showed 90% lymphocytes, indicating a viral cause. Viral screen of the cerebrospinal fluid was negative for herpes, Japanese B, and West Nile viruses.
To investigate other potential causes of her neurological symptoms, an MRI of the brain and cervical spine was conducted on the 10th day after symptoms began. The MRI revealed ill-defined, bilaterally symmetrical, hyperintense areas on T2/FLAIR images involving the basal ganglia, substantia nigra, peri-aqueductal grey matter, and pontine tegmentum, as well as the dorsal aspect of the medulla. Hyperintense lesions were also present in the bilateral posterior thalami and hippocampi. A linear, T2 hyperintensity also extended into the cervical spinal cord, involving the central grey matter. These areas appeared hypointense on T1-weighted images. Diffusion-weighted imaging showed no signs of restricted movement. There was no evidence of blooming or contrast enhancement. The cortical grey matter and white matter in both hemispheres showed normal signal intensity. These findings were consistent with those reported in previous cases of rabies encephalitis.
The patient’s neurological condition continued to deteriorate, necessitating intubation. Unfortunately, 5 days later, the child passed away. Due to the distinct clinical presentation and the swift progression of the disease leading to death, laboratory confirmation was not obtained.
DISCUSSION
Rabies is a severe and often deadly central nervous system (CNS) infection caused by a neurotropic virus belonging to the Rhabdovirus family.3 Typically, it spreads through the bite of a rabid dog, through aerosol transmission in caves inhabited by bats, or through contamination of open wounds or mucous membranes. Rarely, it can also be transmitted through corneal or organ transplantation.4,5 The incubation period ranges from 2–8 weeks and depends on factors such as the amount of virus transmitted and the proximity of the site of bite to the CNS.6,7
The virus first replicates in the muscle tissue, attracted by its affinity for nicotinic cholinergic receptors, before reaching the CNS through the neuromuscular spindles or the motor end plates.6 Alternatively, it can also impact the sensory nerve endings and travel retrogradely into the CNS at a relatively constant rate of 12–24 mm per day.8
After the variable incubation period and prodromal phase, characterised by symptoms like burning, itching, and numbness, patients with rabies develop neurological symptoms. The acute neurological phase involving the CNS presents in two clinical forms: classic encephalitic or furious and paralytic or dumb rabies.3,7,9 The encephalitic form is more common, accounting for approximately 80% of cases.7 The encephalitic and paralytic forms of rabies differ both in their clinical presentations and to some extent in their imaging findings as well.3,9 In the encephalitic form, patients initially exhibit hyperactivity, which progresses to periods of fluctuating consciousness. They may also experience phobic spasms, aerophobia, and hydrophobia, with even the mention of water triggering these hallmark symptoms. In contrast, the paralytic form typically begins with early motor weakness that advances to quadriparesis and facial weakness.3,9,10 In the early stage, the encephalitic form of rabies exhibits a preference for affecting the brainstem and cerebrum, particularly involving the limbic system. Progression of the disease may also involve deep grey matter structures such as the basal ganglia and thalami.3,9,10,11 Additionally, cortical grey matter and white matter can be affected.2 In contrast, paralytic rabies affects the medulla and spinal cord, alongside brain involvement similar to that of the encephalitic form.10,11 Initially, lesions are typically bilaterally symmetrical and are best visualised on T2/FLAIR sequences. In rare cases of rabies survival, chronic stages may show persistent lesions in deep grey matter with areas of demyelination affecting the white matter of cerebral hemispheres, brainstem, and cerebellum.2
There is a paucity of literature on the neuroimaging findings of rabies encephalitis, and despite a thorough literature search, the authors could find only two previous studies mentioning the time of MRI study from the onset of symptoms. The MRI brain findings were mostly reported within 5-8 days of onset of symptoms in these two studies by Rao et al.2 and Jassi et al.12
MRI typically reveals ill-defined and hyperintense lesions on T2/FLAIR images, with corresponding areas appearing hypointense on T1-weighted images. In a case series documented by Jassi et al.12 in 2016, MRI findings revealed ill-defined T2/FLAIR hyperintense lesions in the brainstem, affecting the dorsal medulla, pons, periaqueductal gray matter, midbrain, cerebellar peduncles, including the thalami, hypothalamus, hippocampi, and basal ganglia in a bilaterally symmetrical fashion. A similar pattern of involvement was also reported by Awasthi et al.13 in 2001, Rao et al.2 in 2017, and Jain et al.14 in 2013. In the case reported by Awasthi et al.,13 abnormal T1/T2 hyperintense lesions were observed involving the basal ganglia and thalami, attributed to extracellular methaemoglobin resulting from neuronal damage and petechial haemorrhages. Contrast enhancement is usually absent in the early stages; however, mild-to-moderate enhancement can be observed in lesions affecting the brainstem nuclei, hypothalami, grey matter of the spinal cord, and intradural nerve roots in the cervical region, particularly in later stages when the patient is in a comatose state.15 An exception is seen in the brachial plexus, which may exhibit enhancement during the prodromal phase of the disease.9 While MRI findings of diffusion restriction in rabies are infrequent, it’s important to note that restriction is not characteristic of rabies encephalitis. Nonetheless, a few case reports have documented instances of restricted diffusion in the acute stages of encephalitis.2
Diagnosing rabies becomes more straightforward when a patient presents with encephalitic symptoms. However, in cases like the authors’ where the presentation is in a paralytic form, diagnosis is often delayed due to clinical features resembling other rapidly progressive illnesses such as Guillain-Barré syndrome or acute disseminated encephalomyelitis (ADEM). Guillain-Barré syndrome manifests as an acute inflammatory demyelinating illness with lesions primarily affecting the nerve roots of the cauda equina. Conversely, ADEM typically occurs following viral infections or vaccination and is characterised by large confluent T2/FLAIR hyperintense lesions involving the white matter, along with cortical and deep grey matter involvement.
In this case, a history of dog bite on the face with typical clinical symptoms and absence of confluent lesions in the white matter, along with the preferential involvement of specific areas such as the thalami, basal ganglia, brainstem, spinal cord, and hippocampi, coupled with the rapid progression of the disease, led the authors to the diagnosis of rabies encephalitis.
Definitive diagnosis of rabies requires laboratory confirmation. Traditionally, diagnosis was made through demonstration of viral antigen by direct immunofluorescence test in corneal/conjunctival smears and skin biopsies,16 which otherwise have a low sensitivity. The advent of newer techniques such as RT-PCR has shown increased detection due to higher sensitivity and specificity of ~95–100%.17 However, poor availability of these tests may further delay the confirmation of this fatal illness. In such scenarios, characteristic MRI imaging findings might help in early diagnosis and implementing necessary measures.
CONCLUSION
Rabies, a rare and fatal illness known for its swift disease progression, is seldom subjected to imaging, with only a handful of case reports detailing the imaging findings. Additionally, diagnosing the paralytic form is challenging as it closely resembles other rapidly progressing illnesses clinically. However, demonstrating characteristic imaging findings on MRI, showing classical absence of fluffy, cloud-like white matter lesions may aid in distinguishing it from other forms of encephalitis, especially ADEM.
While early diagnosis of rabies may not significantly alter patient management, timely identification through MRI, as in this case, can facilitate the implementation of early public health measures and ensure proper handling of body fluids and biological tissues. Moreover, pinpointing the animal responsible for disease transmission can prevent further spread of infection to other individuals.







