Abstract
Nerve abscess is an infrequently reported complication of leprosy. It is also an uncommon first manifestation of leprosy. In this case, due to the absence of classic signs and symptoms, such as skin lesions, hypoesthesia, and loss of sensation, the swelling was clinically diagnosed as a peripheral nerve sheath tumour on initial presentation. The authors have described an unusual presentation of pure neuritic leprosy that showcased nerve abscess. Clinical presentation was swelling over the medial aspect of the right arm and ulnar aspect of the right forearm, and clawing of the fourth and fifth digits of the right hand, with no signs of inflammation present on the skin surrounding the swelling. Hansen’s disease with pure nerve involvement could not be considered as a differential diagnosis solely based on clinical examination, therefore posing a diagnostic challenge. On ultrasonography, the right ulnar nerve showed diffuse intermittent thickening and a heterogeneously hypoechoic fusiform area with internal echoes at the site of swelling indicating a nerve abscess. These led the authors to the diagnosis of leprosy with perineuronal abscess. Histopathology confirmed the diagnosis by revealing granulomas and acid-fast Hansen’s bacilli. The patient showed dramatic response to surgery, multidrug therapy, and systemic corticosteroids.
Key Points
1. Nerve abscess should always be kept in the list of differentials before clinically labelling the lesions along the course of a nerve as peripheral nerve sheath tumours.
2. Ultrasound has a key role in prompt imaging diagnosis of nerve abscess in a pure neuritic case of Hansen’s disease and its final confirmation through ultrasound-guided fine needle aspiration cytology.
3. A prime role is played by ultrasound in distinguishing nerve abscess from peripheral nerve sheath tumour, and hence clearing out the dilemma.
INTRODUCTION
Leprosy, also known as Hansen’s disease, is a chronic granulomatous infection. It is non-fatal and slowly progressive. Its causative organism is Mycobacterium leprae.1-11 There is skin involvement in the form of hypopigmented patches and loss of sensation over the affected areas, which commonly include the skin, peripheral nerves, mucosa of the upper respiratory tract, and eyes.2,4-9,11-13 It also involves the peripheral nervous system, mostly in the form of nerve thickening.2-6,8-15 The eyes and testes are highly susceptible to the disease, as they have a lower temperature than the core body temperature.3,4,16 The ability of the organism to invade the nerve sheath and cause immune-mediated reactions gives rise to devitalisation and mutilation promoting coherent psychosocial disruption.2,4,9,11,13,14,17 Based on an individual’s immune status, leprosy presents as a spectrum of diseases, extending from polar tuberculoid in patients with higher immunity to polar lepromatous in patients with the least immunity.1-5,10,14
A characteristic feature of leprosy is the bacterial parasitisation of peripheral nerves.3,9-11,13,17,18 In most cases, a granuloma that is formed may soften to form an abscess. This nerve abscess may rupture through the skin, or may cause persistent pressure on the nerve fibres. Hence, it needs to be incised and drained.19
Patients with leprosy develop nerve abscesses in all forms of the disease, but those with the borderline tuberculoid form are known to commonly develop nerve abscess of the ulnar nerve.1,3,5,12,16,20
In literature, other words used as synonyms for pure neuritic leprosy include neural, neuritic, pure neural, primary neural, primary neuritic, simply neural, and polyneuritic leprosy.5,19,21
This report elucidates the necessity of ultrasonography (USG) in a patient with purely neuritic leprosy. Uniqueness of this report lies in the way ultrasound changed the thought process from the clinical diagnosis of schwannoma to the actual diagnosis of nerve abscess in Hansen’s disease. In addition, ultrasound was also used to confirm the final diagnosis using ultrasound-guided fine needle aspiration cytology.
PATIENT INFORMATION
A 12-year-old, female child came to the paediatric department for a gradually progressive, painless swelling that had developed over the medial aspect of the right arm and ulnar aspect of the right forearm in the past year. There was no history of fever, hypoesthesia, or loss of sensation. There was no past history or family history of any chronic medical, psychiatric, or surgical illnesses, and there was no relevant past medical or surgical intervention.
CLINICAL FINDINGS
On clinical examination, no active lesions or skin nodules were seen at the sites of swelling, or anywhere on the body. The swelling over the medial aspect of the right arm was 3×3 cm, nodular-fusiform, soft, mobile, non-fluctuant, and non-tender. There was no local rise in temperature. The transillumination test was negative and the slip sign was positive. The swelling over the ulnar aspect of the right forearm measured 2×3 cm with similar clinical signs. It was fixed on active wrist flexion. Ulnar claw hand deformity in the fourth and fifth fingers of the right hand with wasting of the thenar and hypothenar muscles, and ‘guttering’ of first web space was observed (Figure 1).
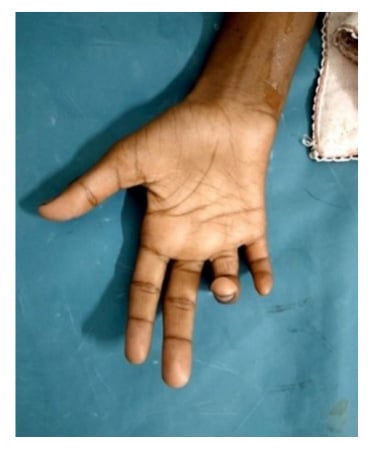
Figure 1: Clawing of the patient’s fourth and fifth fingers.
Clinical image of the patient demonstrating ulnar claw hand with extension at the fourth and fifth metacarpophalangeal joint and flexion at the interphalangeal joint of the fourth and fifth digit, indicating the involvement of the ulnar nerve.
A clinical differential diagnosis of a nerve sheath tumour was made. The patient was advised to perform USG and USG-guided fine needle aspiration cytology of right arm and forearm masses.
DIAGNOSTIC ASSESSMENT
USG with the high-frequency probe revealed multiple intermittent areas of right ulnar nerve thickening with a well-defined fusiform heterogeneously hypoechoic cystic area measuring approximately 3×1 cm at the site of the swelling. It showed internal debris and focal calcification within. There was no internal vascularity within the lesion (Figure 2). The diagnosis of nerve abscess was made.
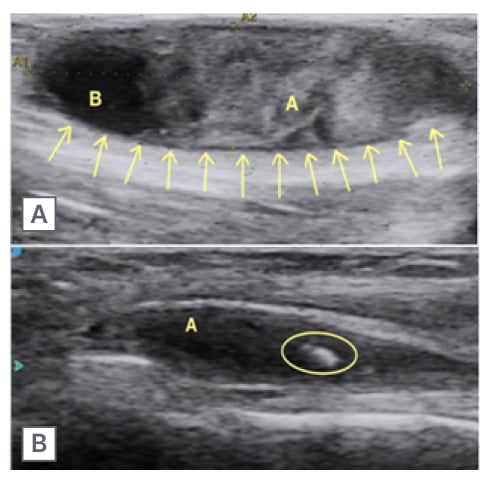
Figure 2: Ultrasound image, and calcific foci in nerve abscess.
A) Longitudinal ultrasound image shows a well-defined heterogeneously hypoechoic fusiform area (marked by arrows) with internal echoes at the site of swelling suggesting of nerve abscess.
1) represents the hyperechoic component within the abscess denoting debris within; and 2) denotes the liquefied component of the abscess.
B) Longitudinal ultrasound image shows a well-defined hypoechoic fusiform area (1) within the ulnar nerve with a focal calcification (within the circle).
USG-guided fine needle aspiration cytology was performed from the swelling (Figure 3). The smears were reported to show neutrophils, lymphocytes, and histiocytes, including foamy histiocytes and epithelioid histiocytes forming an occasional aggregate with the background showing necrosis. On Ziehl–Neelson staining, acid fast tubercle bacilli were not seen. On Fite–Faraco staining, acid fast lepra bacilli were seen. The impression indicated acute on chronic inflammation with focal epithelioid granulomas. They further advised a Mycobacterium tuberculosis workup and slit skin smear examination.
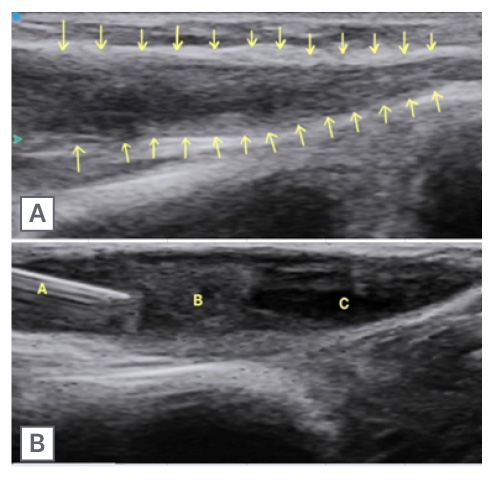
Figure 3: Ultrasound image of ulnar nerve, and ultrasound-guided fine needle aspiration cytology.
A) Thickened ulnar nerve indicated by arrows.
B) Needle tip (1) inside the nerve abscess (2) for FNAC. The hypoechoic area (3) within it denotes the liquefied component of the abscess.
FNAC: fine needle aspiration cytology.
The patient was then referred to the Department of Dermatology and Venereal Diseases in view of Hansen’s disease. On examination, thickening was present in bilateral ulnar, radial, and common peroneal nerves without any tenderness. In addition to this, Froment’s test was positive in the right hand, and Card’s test was positive in the right hand’s fourth and fifth fingers. There was no evidence of ankylosis at the interphalangeal joints, and no signs of inflammation at the site of the lesion. The absence of skin lesions was also confirmed.
THERAPEUTIC INTERVENTION
No skin lesions suggestive of leprosy were noted on complete skin examination. The peripheral nerves were thickened and showed nodular swellings along the course of the right ulnar nerve proximal to the medial epicondyle. There was no reduction in sensations to touch or temperature.
A motor deficit was present, and no sensory manifestation was noted. Slit skin smear examination was negative. Based on all the radiological and clinicopathological findings, surgical exploration of the ulnar nerve aiming for pus drainage, debridement, external neurolysis, and decompression was performed by the Department of Surgery. The patient was started on 6 months of paucibacillary multidrug treatment, including dapsone 100 mg daily and rifampicin 600 mg monthly (supervised) for pure neuritic leprosy. Additionally, systemic corticosteroids (prednisolone) were administered.
FOLLOW-UP AND OUTCOME
The patient did not show any neurological impairment or further progression of the disease. They did not have any adverse effects from the drugs that were administered, and had a full recovery. A timeline of the case is represented in Figure 4.
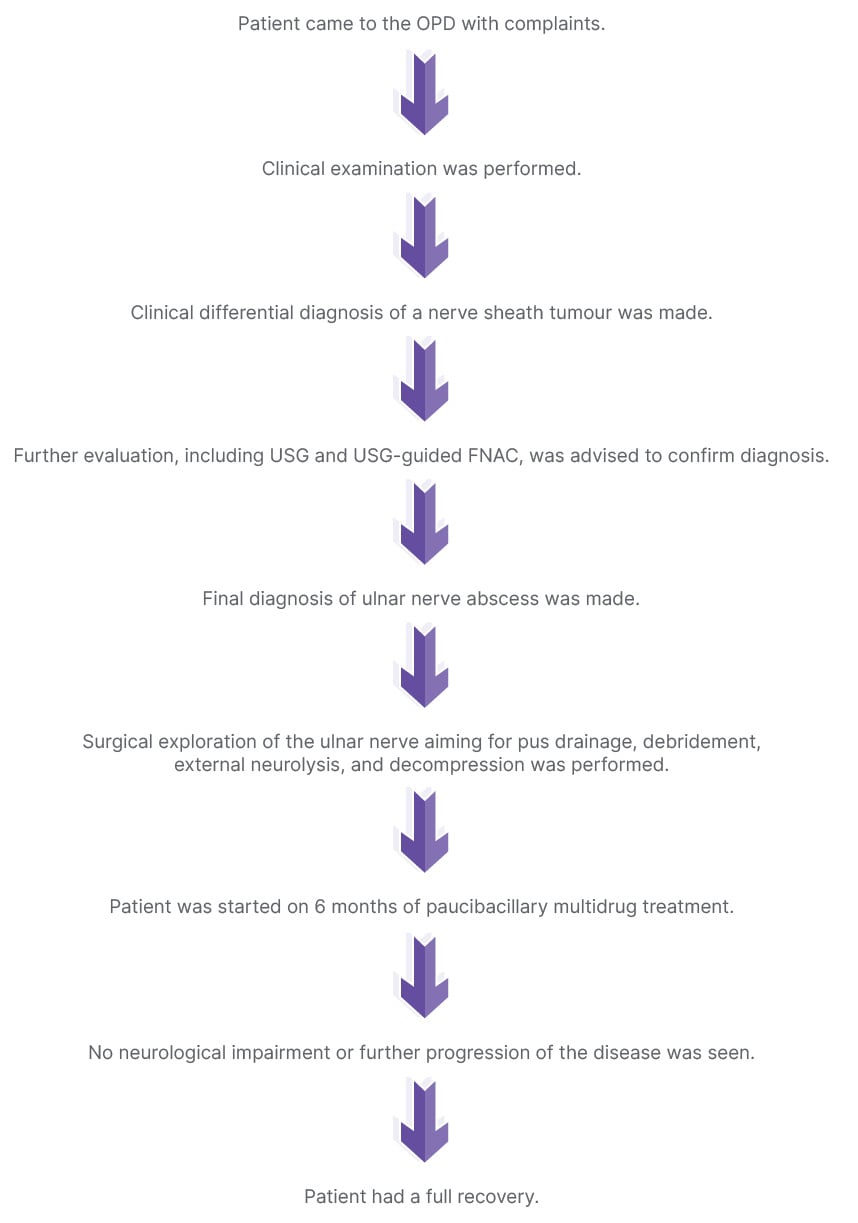
Figure 4: Timeline.
FNAC: fine needle aspiration cytology; OPD: outpatient department; USG: ultrasonography.
DISCUSSION
Leprosy, a disease of bacterial origin, shows haematogenous dissemination or contiguous spread through the skin.3,20 The organism mainly resides in the peripheral myelin forming cells of the nerves, preferably at a site with lower temperature than the core body temperature, sites of injury, or at the site of nerve entrapment in the superficial soft tissue plane, but it can occasionally invade the ensheathed axons.3,18,20 These acid-fast Hansen’s bacilli in the affected nerves undergo restricted multiplication.3,9,10,18 The host immunity recognises the exposed bacterial antigen, thus initiating a granulomatous reaction.3,9 The Schwann cells assume phagocytic function and transform into macrophages or epithelioid cells of the granulomas.3,4,8-10,13,17,18,20,22 These granulomas may become caseous and show areas of necrosis leading to the formation of an abscess. The ulnar nerve is the most common nerve affected in a case of leprotic nerve abscess.5,23 Although nerve abscesses have been accounted in all types of leprosy, their highest occurrence has been noted in borderline tuberculoid leprosy.5,8,14,24-28 Leprotic nerve abscess is an extremely rare manifestation of leprosy, but should always be considered in endemic areas, as in the authors’ case.1,8,14,16,19 In leprosy, nerve abscesses are generally cold abscesses’, as seen in patients with tuberculosis, and are not painful.21 These are ‘silent abscesses’ with no indication of inflammation, and they are easily misdiagnosed as soft tissue mass lesions, neuroma, or lymphadenitis, especially if they appear at an unusual site.21,29-32 The magnitude of subsequent nerve function impairment is not reflected by the size of abscess. Depending on its placement in the nerve, even a tiny intraneural abscess can be linked with severe nerve function impairment.3,21 In the authors’ case, the patient had pure motor symptoms in the form of ulnar claw hand.
Peripheral nerve involvement without any skin lesion, presenting mainly as sensory and motor impairment affecting single or multiple nerves, is characteristic of pure neuritic leprosy.2,3,5,8-10,13,18,23,33-36 Its occurrence is more common in the Indian subcontinent, frequently involving the upper limb nerves, of which the ulnar nerve shows the most common involvement.1,5,14,17,18,21,32
Swelling due to nerve abscess is an uncommon initial presenting symptom of leprosy. To make the correct diagnosis for nerve abscess, a high index of suspicion is required.23,34,37 In cases of leprosy, clinical examination is not always reliable since nerves may not be compliant to palpate.10,11,17,18,23,38 Therefore, amongst all radiological modalities, USG seems to be a more useful and feasible choice for its diagnosis as compared to MRI.2,3,8,11,12,17,18,20,22,32,34,36,39-43 A more useful method for diagnosis is high resolution ultrasound, which enables objective visualisation of nerve enlargement and evaluation of underlying soft tissue, and hence should be the preferred choice in suspected cases of pure neuritic leprosy.2-4,8,10-12,16-18,20,22,23,32-36,38,40-42,44-46 The most important findings of leprosy on high-resolution ultrasound include thickening of the nerves with loss of normal fibrillary pattern.3,4,8,10-12,17,18,20,22,23,32-36,40-43,45,46,48 Increased vascularity on Doppler can be seen.2,3,11,12,18,22,23,34,35,43,44 Sometimes, intermittent thickening of the nerve can be noted.2-4,8,10-12,16-18,20,22,23,32,34-36,38,40,41,44-49 Rarely, perineural and nerve abscesses can be seen, as in the authors’ case. In case of nerve abscesses, USG Doppler can be used to access the absence of vascularity within the lesion to differentiate it from peripheral nerve sheath lesions, which are generally hypervascular.2,3,12,18,22,23,34,38,44
This case emphasises the role of common non-invasive radiological modalities like ultrasound in pinpointing the diagnosis of Hansen’s disease in endemic areas. At the same time, this case presents a learning point that not all nerve lesions are peripheral nerve sheath tumours. A mindful clinical and radiological approach with USG-guided intervention played a huge role in the diagnosis of this rare case, which is a great learning point.
PATIENT PERSPECTIVE
The patient and patient’s parents/guardians chose not to make a statement.
METHODS
The authors’ Institutional Review Board granted exemption for this case report. Written informed consent was obtained from the patient’s parents/guardians as the patient was below 18 years of age. CARE reporting guidelines were used to draft the manuscript of this case report.50







