Abstract
Objectives: Paediatric neuroradiology is one of the most challenging areas in the wide gamut of disciplines that modern radiology encompasses. There is a paucity of literature on the epidemiology of paediatric neuroimaging and contextual reporting in this field. The objectives of this study were to study the epidemiology of the paediatric neurological disorders and to study the role of contextual reporting in this field.
Materials and methods: This study was conducted at a tertiary care centre in Southwestern India over 1 year. It was a retrospective epidemiological study. The authors studied 112 patients referred as in- or outpatients for a brain MRI for a wide range of indications. The authors analysed the reports issued by their radiologists and reformatted them into a newly proposed contextual reporting template for the paediatric brain. Then, the authors conducted an epidemiological analysis of the compiled data.
Results: The authors found that the most common indication for paediatric neuroimaging was seizures or seizure-like episodes, followed by developmental delay. The most common abnormality on imaging was sequelae to hypoxic or hypoglycaemic insult followed by brain atrophy. The authors found a wide range of other abnormalities illustrating the wide spectrum of paediatric neuroradiology.
Conclusion: The authors’ study fills a gap in current literature regarding the epidemiology of conditions encountered in paediatric neuroradiology. The authors also propose a novel reporting format for contextual reporting in this field, which may help in reducing errors in reporting and reduce reporting time.
Key Points
1. Challenges in capturing reliable paediatric neuroimaging mean that accurate reporting is imperative. A better understanding of epidemiological breakdown of indications for neuroimaging can help to direct accurate reporting, particularly when using ‘contextual reporting’ methods.2. This retrospective epidemiological study found that the most common indication for paediatric neuroimaging
was seizures or seizure-like episodes, followed by developmental delay. The most common abnormality observed on imaging was sequelae to hypoxic or hypoglycaemic insult, followed by brain atrophy.
3. Contextual reporting of paediatric neuroimaging, where the structured reporting format is dependent on clinical indication, may improve the speed and accuracy of reporting. The authors of this study provide a suggested template for contextual reporting in paediatric neuroimaging.
INTRODUCTION
Paediatric neuroradiology is one of the most challenging areas in the wide gamut of disciplines that modern radiology encompasses.1 There are numerous challenges to obtaining diagnostic quality images, which range from inherent poor signal-to-noise ratio to patient motion to the rapid changes that are happening in the developing paediatric brain.2
There is a paucity of literature, particularly in the Indian population, on the spectrum of paediatric brain disorders and the value of MRI in their diagnosis. There have been multiple epidemiological studies on specific disease groups, including paediatric brain tumours and neonatal seizures.3,4 However, the authors could not find a study analysing the entire spectrum of neuroimaging findings in this age group. Hence, the primary aim of this study was to dissect the epidemiology of paediatric brain disorders on neuroimaging in a tertiary care centre.
Contextual reporting is an alternative way to report where the reporting format is dependent on clinical indication.5 This approach is finding increasing traction in recent literature.6 The authors explore the role of contextual reporting in paediatric neuroimaging. The authors also endeavor to suggest tailored study protocols, as well as a fresh format for contextual reporting for different indications in paediatric neuroimaging to increase the speed and accuracy of reporting. Hence, this study had two aims: first, to provide an epidemiological distribution of paediatric brain conditions seen on neuroimaging and second, to create a comprehensive template for contextual reporting of the paediatric brain MRIs.
METHODS
Study Population
A total of 112 paediatric patients ranging from 0 years to 18 years of age as per the World Health Organization (WHO) definition of a paediatric patient were studied retrospectively from 1st May 2019 to 31st April 2020.7 These were various inpatients or outpatients who were referred for MRI of the brain for a wide range of indications. The authors included all patients fulfilling these criteria. Most of the patients were examined once during the study period except for a few who underwent follow-up studies. The authors excluded these follow-up studies from the study.
Initial Clinical and Laboratory Evaluation
In addition to the clinical details provided on the requisition forms, detailed perinatal history was collected for all the patients. This included the history of pre-term or post-term delivery, birth asphyxia, admission to neonatal intensive care unit, and history of meconium aspiration. Relevant biochemical and genetic test results were recorded for all the patients. As an institutional protocol, this data is collected and recorded from all patients visiting the MRI centre by interviewing the patients or caregivers and reviewing their documents. The same data was used for this study. Also, the following data were recorded for all patients: age, sex, symptoms, age of their onset, examination findings, and provisional clinical diagnosis.
Equipment and Technique
The MRI examination was performed using a 1.5T Siemens Somatom Symphony MRI machine (Siemens AG, Munich, Germany). The authors followed the institutional magnetic resonance (MR) protocol for brain imaging, which included T1-weighted (W), T2W, T1W inversion recovery, fluid-attenuated inversion recovery (FLAIR), diffusion-weighted imaging, and gradient-recalled echo sequences in the axial plane (T2W sequence in the coronal plane and T1W sequence in the sagittal plane). In selected cases, 3D-T1W- magnetisation-prepared rapid gradient echo imaging, fat-saturated post-contrast imaging, MR angiography, MR spectroscopy, and constructive interference in steady state sequences were employed based on the clinical history and imaging findings on routine sequences. A few patients also underwent simultaneous imaging of the spine.
All MRIs were reported by different radiologists (eight in total) out of which one was a neuroradiologist. The authors included all radiologists in their institute with experience ranging from 2 years to 18 years. Many of the cases were discussed in intradepartmental conferences. The template used for reporting was the same as the adult template with additional remarks on the degree of myelination.
Data Analysis
During data analysis, the authors analysed the narrative reports issued by their radiologists. The authors then reformatted these reports into a newly proposed contextual reporting template for the paediatric brain. The authors designed a fresh template that was inspired from the work of Mamlouk et al.8 Mamlouk et al.8 have suggested four different formats for contextual reporting in the paediatric brain. However, the authors used the spectrum of findings seen in this study to build a single fresh comprehensive template (Table 1), which can serve as a ‘one-stop shop’ for reporting these cases. The authors performed statistical analysis of patient age using MedCalc Statistical Software version 14.8.1 (MedCalc Software, Ostend, Belgium). Descriptive statistics are presented in frequencies and percentages for categorical variables. For continuous variables, means and standard deviations summarise normally distributed data, while medians and ranges summarise non-normally distributed data.
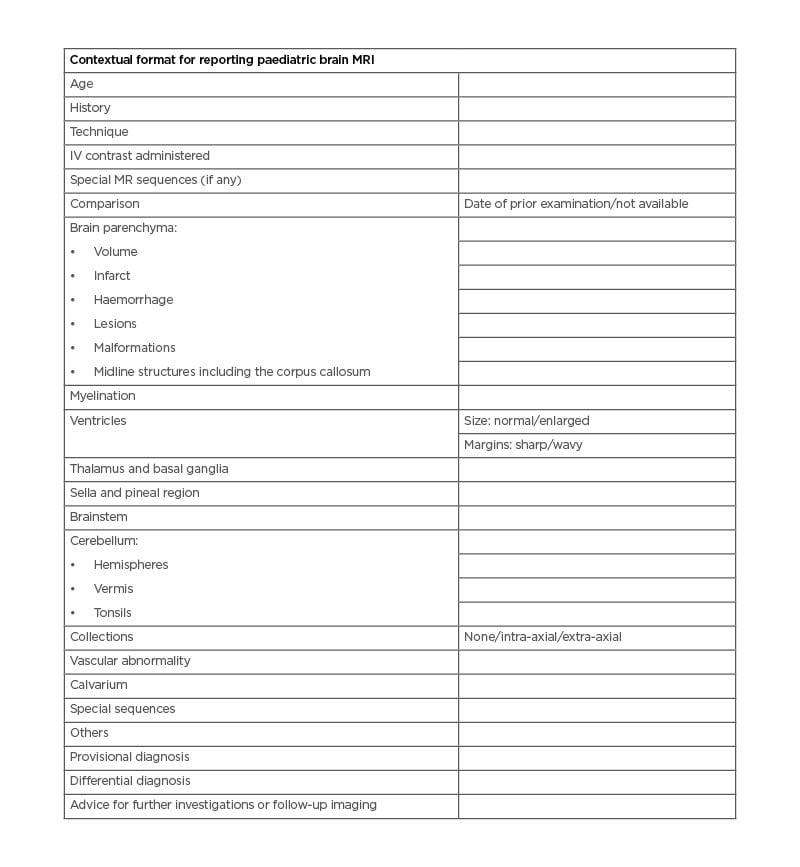
Table 1: Proposed contextual format for reporting paediatric brain MRI.
IV: intravenous; MR: magnetic resonance.
Ethical Considerations
The study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights, and the authors followed the policy concerning informed onsent. The study was approved by the institutional ethics committee of the corresponding authors’ institute. The parents or caregivers of the children reported in this article had signed a written informed consent form. This study was conducted in a medical educational centre, in which all patients are informed that they may be subjects of scientific experiments and are informed of the ethical codes of conduct. This was a retrospective study without active intervention and no enrolment in the public trials registry was required as per the ethical code of conduct of their institute.
RESULTS
Patient Demographics
The study population ranged from age of 7 days to 17 years, with a median age of 6.5 years. There was a predominance of male patients (n=70) compared to female patients (n=43).
Clinical Parameters
In the patient population, 103 patients were born at term, eight were pre-term, and only one patient was delivered post-term. A total of 17 patients had a history of neonatal intensive care unit admission, ranging from 3 days to 21 days. Among these, five patients were born pre-term and one was born post-term. A total of 13 patients had a history of birth asphyxia.
The most common indication for imaging was focal or generalised seizures or seizure-like episodes in 31 patients. This was followed by the developmental delay seen in 28 patients. This included global developmental delay, intellectual disability, loss of acquired milestones, or short stature. Twenty-seven patients presented with haemiparesis or cerebral palsy. A total of 23 patients were grouped under miscellaneous, which included patients presenting with headache, patients on follow-up for malignancies and tuberculosis, patients undergoing brain screening to rule out metastases, and patients with a syndrome. Two patients were suspected of having tuberous sclerosis. None of the patients in the study had undergone genetic or enzymatic studies before imaging.
MRI Findings
The authors analysed the existing reports issued by the radiologists to extract key headings from them. Following this, the authors created a contextual reporting template to attempt an improvement upon one suggested by Mamlouk et al.8 The format prepared and used by the authors is detailed in Table 1.
Brain Parenchyma
Parenchymal volume
The authors found 22 patients to have various degrees of diffuse brain atrophy. One patient had unilateral atrophy of the left cerebral hemisphere. Another patient had unilateral atrophy of the hippocampus.
White matter abnormalities
A total of 27 patients had white matter abnormalities. The most common finding was the presence of abnormal T2/FLAIR white matter hyperintensity. This was most commonly seen in the periventricular region (in 16 patients) and was associated with a paucity of white matter, suggestive of periventricular leukomalacia (PVL). Two of these patients also had FLAIR hyperintensities in perirolandic regions. One patient had isolated involvement in the perirolandic region. One patient was found to have cystic PVL. Two patients showed white matter hyperintensities, with the corresponding restriction of diffusion. Based on clinical findings, one of these was suspected to be acute demyelination, whereas the findings were presumed to be due to hypoxic white matter injury in the second patient. These were the primary differential diagnoses offered by the reporting radiologists after clinical–radiological correlation. A total of four patients showed asymmetrical white matter hyperintensities, which followed no particular patterns and were suspected to be sequelae of seizures or demyelination. One patient showed radial migration lines and was confirmed to have tuberous sclerosis.
Infarcts
The authors found one patient with acute infarcts and 10 patients with chronic infarcts. The middle cerebral artery territory was the most commonly involved vascular territory.
Haemorrhages
There was only one case of right periventricular haemorrhage. This patient also had cortical laminar necrosis in bilateral perirolandic regions. Two of the patients had haemorrhagic cortical contusions with a history of preceding trauma.
Focal lesions
Four patients had intraparenchymal lesions. Two of these had multiple ring-enhancing lesions (Figures 1A and 1B) and one had a calcified lesion in the right parietal lobe, which likely represented a calcified granuloma (Figures 1C and 1D). One patient had periventricular calcifications with associated findings representing congenital cytomegalovirus infection.
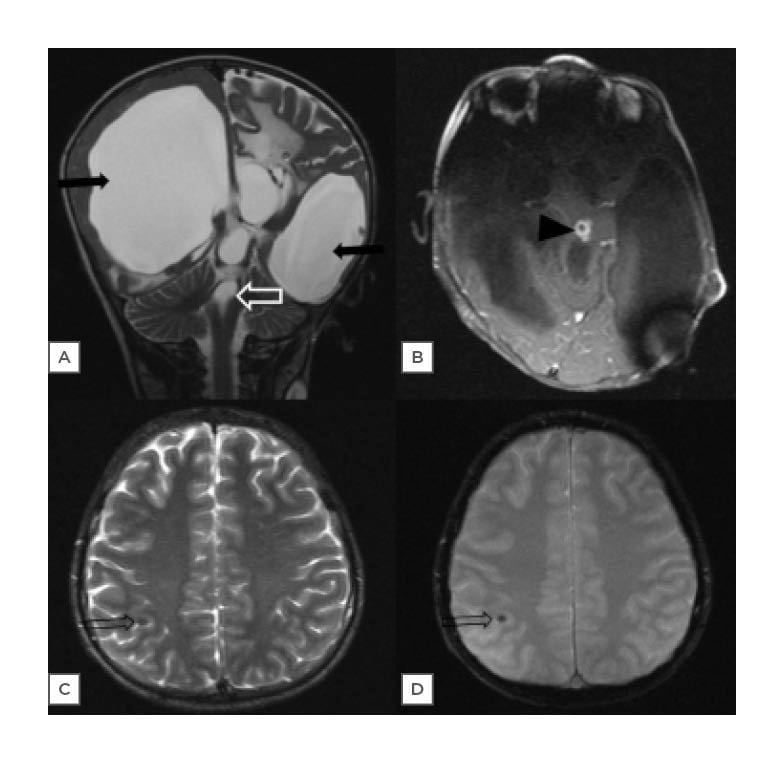
Figure 1: Spectrum of intracranial infections.
A) This MRI brain image of a 1-year-old male shows the presence of gross dilatation of bilateral lateral ventricles and third ventricle (solid black arrows), with normal-appearing fourth ventricle (white void arrow) on T2W coronal images, suggestive of non-communicating hydrocephalus. B) A T1W post-contrast axial image shows an enhancing nodular lesion in the midbrain (black arrowhead). C) An MRI brain image in a 15-year-old male, who presented with seizures, show a punctate focus of hypointensity (void black arrow) on T2W axial. D) Gradient echo axial images, which is likely to represent a calcified infective granuloma.
W: weighted.
Malformations
The study population had six patients with structural malformations. Two of them had cortical tubers and turned out to have tuberous sclerosis. One patient had Type II focal cortical dysplasia with nodular heterotopia. The other three patients had ulegyria, lissencephaly, and pachygyria polymicrogyria complex, respectively.
Midline structures
All 22 patients with diffuse brain atrophy had various degrees of associated corpus callosum atrophy. Besides, two patients had corpus callosum atrophy with preserved brain volume. One of them had associated lissencephaly, whereas others had findings representing PVL.
Myelination
There were four patients with abnormal myelination, which did not correspond to their age. One of these had delayed myelination in the frontal and parietal white matter along with diffuse cerebral atrophy. Another patient had findings representing hypomyelination (T2 hyperintensity of white matter, with a relatively normal signal on T1W image) at the age of 7 years. The other two patients, aged 12 years and 5 years, had diffuse white matter signal abnormality, with the onset of symptoms at age of 4 years and 2 years, respectively, leading to a provisional diagnosis of a demyelinating disorder.
Ventricles
In the study population, 11 patients had ventricular abnormalities. Five of these had a communicating pattern of hydrocephalus, with causes ranging from Chiari II malformation to congenital cytomegalovirus infection. One patient had a ring-enhancing lesion in the mid-brain leading to aqueductal stenosis and resultant obstructive hydrocephalus (Figures 1A and 1B). One patient with a history of trauma had an intraventricular haematoma. Two patients had asymmetric ventricular dilation after placement of ventriculoperitoneal shunt. Interestingly, one of these had multiple 1–2 mm sized enhancing lesions along the ventriculoperitoneal shunt in the left parietal lobe, which likely represented foreign body granulomas. Lastly, two patients with tuberous sclerosis in this study had subependymal nodules.
Thalamus and Basal Ganglia
The authors found six patients with a varying spectrum of findings in basal ganglia. Three of the patients had gliosis and encephalomalacia. One patient had a haemorrhage in the right thalamus, whereas another patient showed restriction of diffusion in bilateral thalami and basal ganglia (with similar findings in white matter due to hypoxic injury). The last patient had calcification in the right basal ganglia, which in conjunction with his other findings, led to the diagnosis of congenital cytomegalovirus infection.
Sella and Pineal Region
The authors found two patients with sellar abnormalities. The first patient, with a known case of Langerhans cell histiocytosis, had a loss of posterior pituitary bright spot. The second patient had partial empty sella. No abnormality of the pineal region was seen.
Brainstem
The authors found one patient with gliotic changes in the vascular territory of the right superior cerebellar artery, representing the sequalae to previous ischaemic insult. Another patient had a ring-enhancing lesion in the mid-brain leading to hydrocephalus, as described above (Figures 1A and 1B).
Cerebellum
Previously described 22 cases of diffuse cerebral atrophy also showed various degrees of cerebellar atrophy. Also, one patient had isolated severe cerebellar atrophy and was suspected to have neuronal ceroid lipofuscinosis. One patient with Chiari II malformation had low-lying peg-shaped tonsils and another patient had tonsillar ectopia without additional abnormalities. No abnormalities of the cerebellar vermis were seen.
Collections
One patient had epidural and subdural collections showing restriction of diffusion and representing abscesses. Another patient with a history of trauma had a subdural haematoma.
Calvarium
The authors found three patients with microcephaly and another patient with occipital bone osteomyelitis.
Special Sequences and Screening of Neuraxis
The authors performed MR angiography, MR venography, single-voxel MR spectroscopy, and T1, T2, and short tau inversion recovery sagittal sequences for the screening of spinal cord in selected cases. These sequences did not reveal any significant findings.
Other Findings
The miscellaneous findings were found in 15 patients and included entities such as cavum septum pellucidum (n=2), mega cisterna magna (n=3), otomastoiditis (n=1), pansinusitis (n=1), encephalocele (n=1), scalp haemangioma (n=1), and cleft palate (n=1). The patient with elongated and tortuous intracranial vessels was suspected to have Menkes disease.
Provisional Diagnosis
The authors had 41 cases with an impression of ‘normal study’ or ‘no significant abnormality’. The remaining 81 cases had a wide spectrum of provisional diagnoses. These are listed in the pie chart in (Figures 2 ).
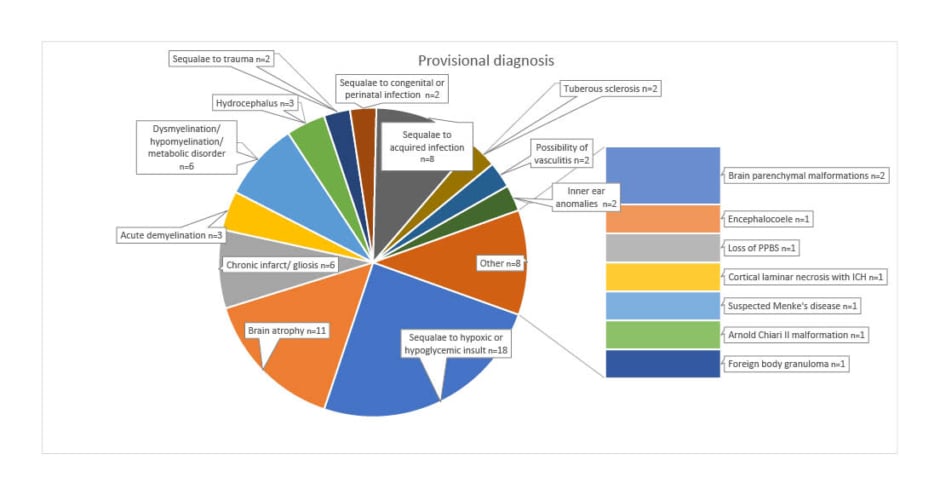
Figure 2: Provisional diagnoses in the study population.
ICH: intracerebral haemorrhage; PPBS: posterior pituitary bright spot.
DISCUSSION
Paediatric neuroimaging continues to pose enormous challenges to radiologists across the spectrum from trainee residents to consultants. There are few studies citing workload devoted to paediatric neuroimaging in tertiary care setups. Cowan et al.9 reported that paediatric neuroimaging makes up for approximately 3% of total MRI examinations.
There have been few studies on the epidemiological distribution of paediatric brain conditions on neuroimaging. Most of these are focused on selective groups of diseases like brain tumours, epilepsy, or neural tube defects.3,4,10 This study tries to fill this information gap by providing a breakdown of all the paediatric brain conditions seen on imaging. This would assist in better understanding of the incidence and distribution of various MRI findings in paediatric neuroimaging.
The most common finding in the analysis was the presence of features of hypoxic or hypoglycaemic brain injury seen in 16% of the study population. The authors grouped these two entities together as there is a wide overlap in imaging findings of these conditions. The reported incidence of hypoxic injury in the literature is 2–6 per 1,000 live births.11 The authors study reflects a higher incidence, which can be attributed to the fact that they only included children referred for neuroimaging.
This was followed by the presence of brain atrophy in 9.8% of the study population without any other abnormality. This a known phenomenon that many paediatric patients show brain atrophy without other clues on MRI. This group usually has a high probability of genetic abnormalities.12
Another objective of this study was to explore the role of contextual reporting in this field. This was achieved by breaking down the existing reports to extract their key findings and then using them to design a fresh template that can be used across all cases of paediatric neuroimaging. Contextual reporting is a form of structured reporting that entails using a reporting format that is tailored towards a particular disease or related group of diseases.8 This differs from structured reporting where reporting formats are set for a particular organ system. Contextual reporting provides focused content related to the particular disease and offers a checklist for all pertinent points required to answer the clinical question.13-15
The inherent challenges in paediatric neuroimaging render it near impossible to perform additional imaging in the event of a missed finding on the preliminary review (while the scan is going on). The primary reason for this is a need for general anaesthesia or heavy sedation in most of the cases for performing MRI.2,16
For example, if a small lesion is missed in the sella during the preliminary review and the scan is completed without administering the contrast, a repeat scan may be required to evaluate contrast uptake of the lesion. Although MRI is a non-ionising modality, such a scan requires repeat sedation, which has its own inherent risks.17 This makes it imperative that radiology trainees use a standardised format for the preliminary review of the images while the patient is inside the gantry. This would also help in adding sequences tailored to a particular condition. This approach has been shown to reduce error rates and reduce reporting times.18
Mamlouk et al.8 have done pioneering work in creating approximately 50 templates for reporting in neuroradiology. The authors selected paediatric neuroradiology from this wide spectrum for the reasons discussed above. The authors suggest a contextual reporting template for paediatric brain imaging to attempt and further improve upon their work (Table 1).
The authors’ template covers a wide range of possible abnormalities encountered in paediatric neuroradiology. The authors used the spectrum of findings in this study to build a comprehensive format that can serve as a one-stop shop for reporting these cases. The contextual reporting format also enables the treating physician by presenting the findings in a structured format. This would help in patient management.
The authors acknowledge the limitations of this study in the form of a relatively small sample size, lack of follow-up examinations for the study group to evaluate the temporal change in studied parameters, and the lack of genetic data. The authors consider this study to be one of the building blocks in the rapidly emerging trend of contextual reporting. In the future, these templates can be integrated with clinical, biochemical, and genetic data leading to data integration and improved patient management. These templates also enable epidemiological research and deep learning.19,20
CONCLUSION
In conclusion, this study fills a gap in current literature regarding the epidemiology of conditions encountered in paediatric neuroradiology. The authors also propose a novel reporting format for contextual reporting in this field, which may help in reducing errors in reporting and the reporting time.