BACKGROUND AND AIMS
The severe acute respiratory syndrome coronavirus 2 pandemic has already infected millions of people worldwide, with 5–10% of cases leading to severe pneumonia. Although the majority improve over time, some patients may progress to post-COVID-19 interstitial lung disease. The aim of this abstract review was to investigate the characteristics of post-COVID-19 interstitial lung changes, with the unique opportunity to evaluate radiologic–pathologic correlations using high-resolution chest CT (HRCT) and transbronchial lung cryobiopsy specimens.
MATERIALS AND METHODS
The authors used preliminary results of HRCT features of post-COVID-19 interstitial lung disease. The authors collected data of hospitalised patients at baseline, then at 6 (±1) months and 12 (±1) months after discharge. HRCT changes at 6 months involving more than 5% of the total lung volume were considered significant, following the current definition of interstitial lung abnormalities. Thoracic radiologists were asked to define each HRCT as negative for pleural and parenchymal alterations, or if positive, whether alterations were predominantly fibrosing-like or non-fibrosing-like. Patients with significant HRCT changes underwent bronchoalveolar lavage and/or cryobiopsy, and a subsequent follow-up with HRCT and lung function evaluation at 18 (±1) months.
RESULTS
At the time of the present interim analysis, 139 patients from the Careggi University Hospital, Florence, Italy, were enrolled. Median age was 67 years (range: 18–87 years), and 85 were males (61.1%). At 12-month follow-up, HRCT significant changes (both fibrotic-like and non-fibrotic-like) were detected in 53 subjects (38.1%). Of these, only 2/53 (3.8%) patients had parenchymal progression of the disease. There was stability in 33/53 (62.3%) and improvement of lung involvement in 18/53 (33.9%). Cryobiopsies were performed in 10 patients, showing some discordance with radiological appearance (Figure 1). In particular, biopsy found two cases of histological usual interstitial pneumonia (UIP)/early UIP, where HRCT demonstrated a non-specific interstitial pneumonia (NSIP)/organising pneumonia (OP) pattern. Cryobiopsy confirmed one case of HRCT UIP-probable pattern, and three cases of NSIP/OP/hypersensitivity pneumonitis pattern. Moreover, histological evaluation confirmed the radiological pattern found in two cases of early fibrosing disease related to COVID-19 infection, and in two cases of fibrosing ventilator-associated lung injury.
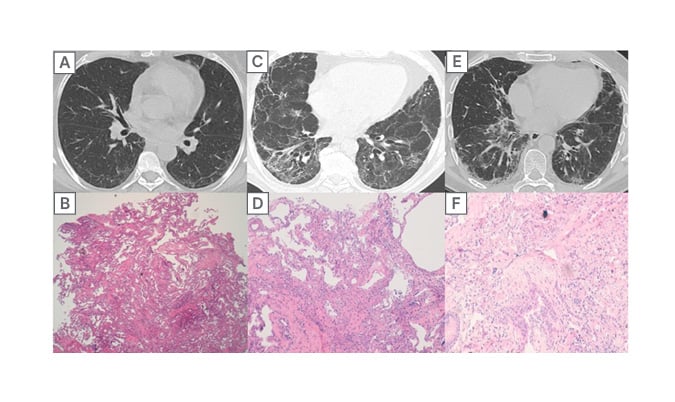
Figure 1: 12-month follow-up high-resolution chest CT and correlation with histology.
Case 1 (A-B): HRCT 12-month follow-up with an indeterminate-pattern fibrosis. (A) Biopsy specimen shows homogeneous septal thickening with initial fibrosis and dilatation of the interstitial capillaries. Initial inflammatory infiltrate in the peribronchiolar area, classified as indeterminate fibrosis. (B) In this case, multidisciplinary decision was post-COVID-19-related fibrosis. Case 2 (C-D): 12-month follow-up HRCT with a fibrosing NSIP/OP pattern and diffuse bronchial distortion. (C) Histological evaluation demonstrates the presence of dense and diffuse fibrosis, mild interstitial inflammation, with prominent bronchiolar damage (epithelial damage including epithelial detachment and alveolar denudation). (D) This is a case of ventilator-associated lung injury. Case 3 (E-F): HRCT with a probable UIP pattern. (E) Confirmed also with the biopsy showing dense patchy fibrosis with microscopic honeycombing and a fibroblastic foci. (F) Multidisciplinary decision was pulmonary fibrosis, and the patient started antifibrotic therapy.
HRCT: high-resolution chest CT; NSIP: non-specific interstitial pneumonia; OP: organising pneumonia; UIP: usual interstitial pneumonia.
CONCLUSION
This preliminary analysis confirmed that after COVID-19 infection, a minority of patients developed interstitial lung changes, mostly with an NSIP/OP or (early) UIP pattern. The UIP pattern found in this study could be the expression of a pre-existing non-diagnosed lung fibrosis or idiopathic pulmonary fibrosis. The hypothesis is that the infection could be a trigger for a possible underlying latent interstitial disease in predisposed subjects.
LIMITATIONS
This study used a small sample size of patients with fibrotic-like changes (without histologic confirmation), which may need a longer follow-up to determine whether the fibrotic-like changes are permanent, progressive, or reversible.








