BACKGROUND AND AIMS
Liver transplantation is the primary treatment for patients with early-stage hepatocellular carcinoma (HCC), which is not eligible for resection.1 However, even when Milan criteria are met, disease recurrence occurs in up to 16% of cases, resulting in a decrease in disease-free survival to 40%.2
Therefore, having preoperative knowledge of the likelihood of recurrence would assist in selecting the most suitable liver transplant recipients, potentially avoiding unnecessary surgeries, and improving patient prognosis and organ allocation. In this context, radiomics, which involves high-throughput data extraction from medical images, holds great promise.3 However, there is ongoing debate regarding the optimal data selection strategy, as factors such as the choice of contrast phase and volume of interest (VOI) can significantly impact radiomic analysis results.4-6 Therefore, the authors’ study aimed to investigate how these factors influence radiomic features (RF), to identify the optimal combination for predicting HCC recurrence in liver transplant candidates.
MATERIALS AND METHODS
Liver transplant candidates from 2010–2019, with waitlist placement CT scans showing nodules suspicious for HCC, according to the Liver Reporting and Data System (LI-RADS) criteria7 (LR-4/-5), and histologically confirmed after the transplant, were retrospectively included. Patients who had previously undergone locoregional procedures, exhibited tumour in vein, or had poor image quality were excluded from the analysis. HCC nodules were contoured across arterial, venous, and delayed phases, with or without peritumoral region of 5, 10, and 15 mm. An area of ‘background’ liver parenchyma, distant from the lesions, was also segmented in each phase.
A total of 107 RFs, both directly extracted from segmentations, and normalised for the ‘background’ parenchyma, were obtained using PyRadiomics (Python Software Foundation, Beaverton, Oregon, USA). The normalisation was conducted by calculating the ratio between the RFs extracted from the VOI, and those extracted from the background segmentation. These features were then compared with each other for inter-VOIs and inter-phase relative change, while autocorrelation was assessed using Spearman’s rank correlation coefficient. RFs with relative change <10% and rank correlation coefficient >0.90 were considered non-informative. Informative RFs with different distribution in patients with and without post-transplant recurrence were selected to build multiple logistic regression models. Prediction of post-transplant recurrence was assessed by comparing the areas under the curve from receiver operating characteristic analysis and goodness-of-fit, expressed as the value range of Tjur’s, McFadden’s, and Nagelkerke’s R2.
RESULTS
The CT scans of 53 patients were selected, resulting in a total of 1,032 segmentations from 86 nodules, with eight (15%) recurrence cases. When varying VOIs and phases, the proportion of noninformative RFs, indicating insignificant differences between the VOI and liver background, were 14–26% and 16–34%, respectively, while 4% of RFs showed autocorrelation >0.90.
The selected informative RFs allowed the building of eight predictive models with adequate performance and goodness-of-fit, each comprising 5–12 RFs, with an area under the curve of 0.77–0.90 (p<0.02) and pseudo-R2 values of 0.13–0.46. A predominance of models derived from the arterial phase was observed, utilising the nodule with or without a 5 mm peritumoral region as the VOI, followed by the venous phase, including a 10–15 mm margin after normalisation (Figure 1).
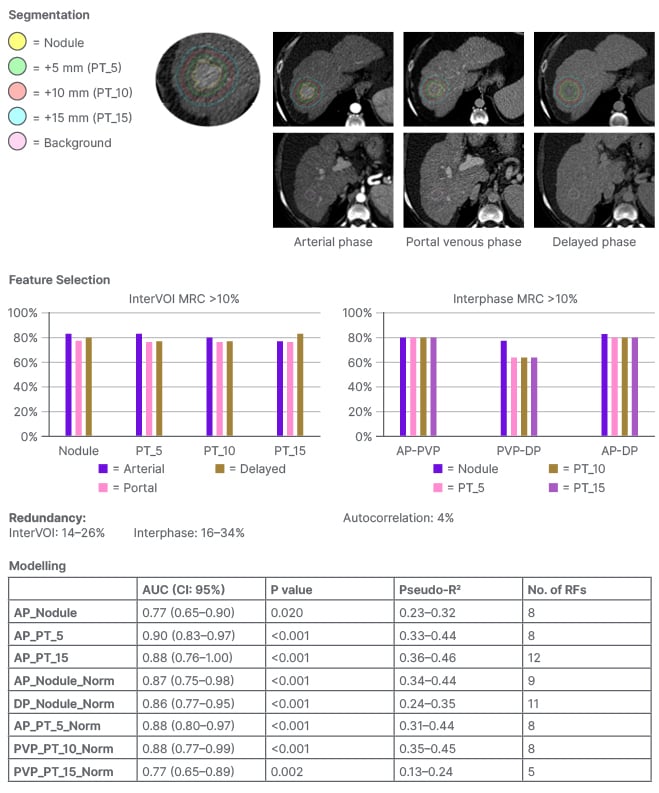
Figure 1: Workflow and results from the radiomic analysis of hepatocellular carcinoma nodules and peritumoural regions extracted from the waitlist placement CT scans of liver transplant candidates to predict disease recurrence.
AP: arterial phase; AUC: area under the curve; CI: confidence interval; DP: delayed phase; No: number; PVP: portal venous phase; RF: radiomic features.
CONCLUSION
Selection of optimal VOI and contrast phase combination is critical to maximise post-liver transplant HCC recurrence prediction using quantitative CT imaging. Specifically, segmenting the nodule, eventually including a 5 mm peritumoral region, during the arterial phase, or the nodule with a 10-15 mm margin during the venous phase after normalisation against the liver background, appeared to be the most promising strategy.







