BACKGROUND AND PURPOSE
Bone is the most common site of metastasis in metastatic breast cancer (MBC), yet no standardised imaging method accurately assesses treatment response.1 CT has limitations in evaluating bone metastases, while RECIST 1. considers bone lesions non-measurable without soft tissue involvement. Bone scans (BS) can produce misleading ‘flare’ reactions, and 18-Fluoro-deoxyglucose (FDG)-PET/CT may miss inactive bone metastases.2 Whole-body MRI (WB-MRI) is emerging as the most effective imaging tool, offering superior sensitivity without ionising radiation or contrast agents.3-6 Additionally, radiology contributes to global greenhouse gas emissions,7 making sustainable techniques8,9 like WB-MRI crucial for reducing environmental impact while ensuring diagnostic accuracy.
This study aimed to measure the energy consumption and greenhouse gas (GHG) emissions of various imaging modalities, aiming to determine the most sustainable and effective option for patients with MBC. The findings could help develop a model for radiology departments worldwide to balance clinical effectiveness with environmental sustainability.
METHODS
Seventy-eight patients with MBC who underwent imaging between 2019–2024 were analysed. Three diagnostic pathways were compared:
- WB-MRI (diagnostic line [DL] 1): Non-contrast imaging with sagittal and axial sequences.
- FDG-PET/CT (DL2): Imaging with a PET/CT scanner following glucose level assessment.
- BS with CT chest-abdomen-pelvis (CT-CAP; DL3): Bone scintigraphy combined with contrast-enhanced CT of the chest, abdomen, and pelvis.
Total scan time (T-Total) was converted into hours to facilitate energy consumption and GHG emission calculations.10 Data were compared across individual imaging modalities and grouped diagnostic lines (DL1, DL2, DL3).
Binary comparisons of scan times, energy consumption, and GHG emissions were conducted using T-test. Average dose values for CT-CAP, FDG-PET/CT, and BS, along with average contrast agent administration data, were calculated.
FINDINGS
Scan Times
DL2 had the shortest mean scan time (0.27 hours), followed by DL1 (0.37 hours) and DL3 (0.56 hours).
Energy Consumption and GHG Emissions
DL2 was the most energy-efficient (4.92 kWh/patient), while DL1 (11.10 kWh) and DL3 (12.05 kWh) consumed significantly more. DL2 reduced emissions by 55% compared to DL1 and DL3 (Figure 1).
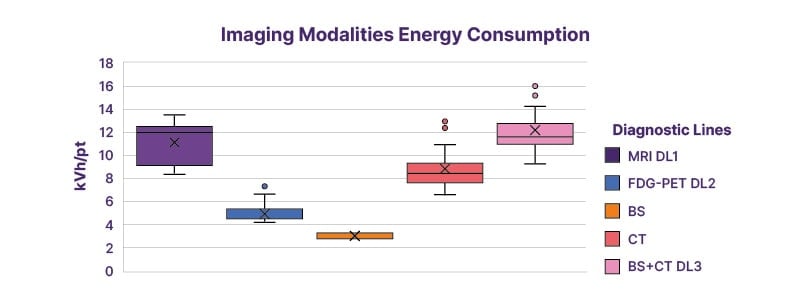
Figure 1: Estimated imaging energy consumption for DL1, DL2, total and individually for DL3 (Bone scans and CT chest-abdomen-pelvis).
BS: bone scan; DL: diagnostic line; FDG: 18-fluoro-deoxyglucose.
Radiation Exposure and Contrast Use
WB-MRI (DL1) had no radiation exposure or contrast media use, unlike DL2 and DL3. FDG-PET/CT (DL2) and BS/CT-CAP (DL3) involved high radiation doses and radiopharmaceutical injections.
CONCLUSION
The new horizons of advanced imaging techniques, especially in oncology, will increasingly have to consider not only the aspect of diagnostic accuracy but also the energy sustainability and biological costs.
These results emphasise the importance of seeking the best and most innovative diagnostic approaches to balance diagnostic accuracy with energy efficiency and biological sustainability. Such advancements could help not only radiology departments become greener but also ensure that patients receive quality and sustainable care.







