BACKGROUND AND AIMS
Anterior ischaemic optic neuropathy (AION) is the most common acute optic neuropathy in older patients. Its annual incidence is 2.3–10.2 cases per 100,000 persons over 50 years. AION can be classified into non-arteritic, accounting for 95% of AION cases, and arteritic, which is mainly associated with giant cells arteritis. Early and accurate diagnosis is essential to avoid severe and irreversible complications such as permanent visual loss.1
The objective of the authors’ study was to assess the impact of timing from onset of visual symptoms to diffusion-weighted 3 Tesla (T) MRI completion to detect ischaemic changes of the optic disc and optic nerve in patients with AION.
MATERIALS AND METHODS
This institutional review board-approved retrospective single-centre study included 3T MRI data from 126 patients with AION and 111 controls with optic neuritis, who were treated between January 2015 and May 2020. Two radiologists, blind to all data, individually analysed imaging. A senior neuroradiologist resolved any discrepancies by consensus. The primary judgment criterion was the restricted diffusion of the optic disc and/or the optic nerve assessed subjectively on the apparent diffusion coefficient (ADC) maps. ADC values were also measured. Spearman’s rank correlation coefficients were used to examine the relationships between timing from onset of visual symptoms to MRI completion, and both the restricted diffusion and the ADC values.
RESULTS
A total of 126 patients (47 [37.3%] were females and 79 [62.7%] were males; mean age: 69.1±13.7 years) with AION were included. Restricted diffusion of the optic disc in eyes with AION was more frequent in the early MRI group than in the late MRI group (35 out of 49 [71.4%] eyes versus three out of 83 [3.6%] eyes, respectively; p<0.001 [ Figure 1 ]). ADC values of the pathological optic discs and optic nerves were lower in the early MRI group than in the late MRI group (0.61 [0.52–0.94]x10-3 mm2/s versus 1.28 [1.01–1.44]x10-3 mm2/s; p<0.001 and 0.74 [0.61–0.88]x10-3 mm2/s versus 0.89 [0.72–1.10]x10-3 mm2/s; p<0.001, respectively).
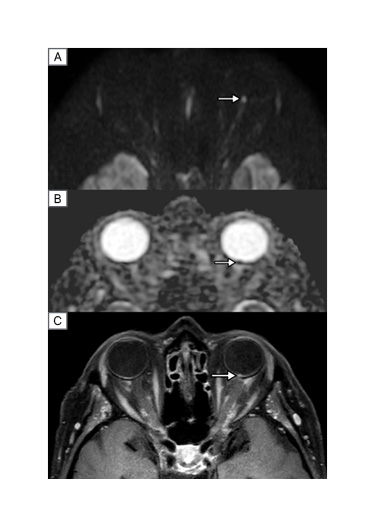
Figure 1: MRI of an 86-year-old female presenting to the emergency department for acute visual loss of the left eye.
MRI was performed 3 days after the onset of visual symptoms. In the left optic disc (arrow), diffusion-weighted MRI (A) shows high signal intensity and ADC map (B) shows reduced ADC value as sign of restricted diffusion. Post-contrast T1-weighted imaging (C) shows enhancement of the left optic disc (arrow). A diagnosis of arteritic anterior ischaemic optic neuropathy of the left eye was confirmed.
ADC: apparent diffusion coefficient; T: tesla.
To the best of the authors’ knowledge, this study was the first one to show a correlation between successfully detecting ischaemic changes in AION and the timing from the onset of AION to the completion of MRI.2 Restricted diffusion of the optic disc was observed in the majority of eyes with AION in the early MRI group, but only rarely in the late MRI group. The authors showed that a threshold of 5 days was optimal to detect ischaemic changes of the optic disc or optic nerve in AION. It highlights the need to perform an MRI as soon as possible to be able to detect ischaemic changes of the optic disc or optic nerve in patients with a suspected diagnosis of AION.
Based on the authors’ results, although a simple visual evaluation of ADC map might be challenging and subjective, an ADC measurement should be systematically performed to confirm a restricted diffusion of the optic nerve or optic disc. Based on the authors’ receiver operating characteristic curves, they provided an optimal ADC threshold of 0.63 for the optic disc to detect AION, yielding a specificity of 95%. This threshold might be used easily in clinical practice.
CONCLUSION
The authors’ results have the potential to modify the management of patients with a suspected diagnosis of AION. Fast-track pathways, including emergency access to an MRI examination, should be considered for diagnosing patients with a suspected diagnosis of AION.3-5
In conclusion, diffusion-weighted MRI showed good diagnostic performance to detect AION when performed early after the onset of visual symptoms.








