BACKGROUND AND AIMS
Dynamic myocardial CT perfusion (CTP) is a relatively novel technique that can depict myocardial ischaemia. However, the radiation dose required for dynamic CTP remains relatively high. Therefore, the authors investigated the feasibility of dose reduction in dynamic myocardial CTP by comparing the diagnostic performance resulting from acquiring images during all heartbeats to that involving the periodic skipping of imaging during a certain proportion of heartbeats.
MATERIALS AND METHODS
The imaging data of 38 patients who presented at the authors’ hospital with chest pain and underwent dynamic CTP on clinical indication were retrieved. All images were acquired with a 320-slice wide-area detector clinical CT system (Aquilion ONE PRISM, Canon Medical Systems Corporation, Ōtawara, Japan), and reconstructed using a deep learning-based algorithm (AiCE Cardiac, Canon Medical Systems Corporation). From the retrieved datasets, three new datasets were created in which every fourth, third, or second beat (i.e., Skip 1:4, Skip 1:3, and Skip 1:2, respectively) were removed as a surrogate of dose-reduced variants of the full-dose protocol. All datasets were post-processed using a dedicated analysis workstation.
Seven radiologists with varying expertise evaluated the reconstructed CT images and perfusion maps in terms of the presence or absence of perfusion deficits per case, providing both a binary decision and a probability of deficit present rating. The latter was used to construct a receiver operating characteristics curve. The mean blood flow (MBF) in each of the 16 myocardial segments was quantified and compared per skipped-beat level, normalised by the respective MBF value for the full-dose (i.e., no skipped-beat acquisition) averaged across patients, and analysed with the analysis of variance. The number of segments and cases whose MBF was below unity (<1.0 mL/g/min) for any acquisition protocol was counted.
Additionally, the authors noted the number of maps with perfusion deficits corresponding to the stenosis on invasive coronary angiography, according to the American Heart Association (AHA) segment model. They also noted the number of non-diagnostic MBF maps (>4 mL/g/min).
RESULTS
No difference was detected in the area under the curve (AUC) based on the radiologists’ probability of deficit present score across datasets (p=0.44; all beats AUC: 0.73; Skip 1:4 AUC: 0.72; Skip 1:3 AUC: 0.76; Skip 1:2 AUC: 0.75) with good observer agreement (intraclass correlation coefficient: 0.8) among the readers. The average relative normalised MBFs (mean absolute error) across reconstructions were: 1.02 (0.11), 1.03 (0.17), and 1.06 (0.20) for Skip 1:4, Skip 1:3, and Skip 1:2, respectively (p=0.66). Overall, 80% of perfusion maps (12 out of 15) showed hypoperfused regions corresponding to the coronary pathology (stenosis, dissection, and occlusion) and 20% of maps (three) had non-diagnostic MBFs across all reconstructions.
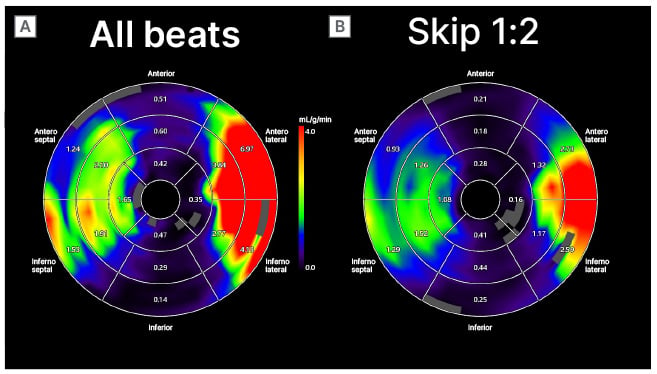
Figure 1: Comparison of the perfusion maps from all beats acquisition (A) and acquisition with skipped every second beat (B).
CONCLUSION
Skipping beat acquisitions, including skipping every second beat, during dynamic myocardial CTP appears feasible. Radiologist diagnostic performance did not decrease after reducing dose by removing 50% of time points in the dynamic sequence, suggesting the possibility of effective radiation dose reduction in dynamic myocardial CT perfusion imaging.








