Abstract
This paper explores the overlooked influence of food insecurity on cancer care, its correlation with malnutrition and poor patient outcomes, and potential strategies for intervention. Food insecurity, the inconsistent access to nutritionally adequate food, significantly impacts up to 55% of patients with cancer, particularly among minority populations, and those of lower socioeconomic status. This multidimensional issue contributes to malnutrition, impairs treatment adherence, and increases mortality rates among patients with cancer. It also exacerbates health disparities, and is intricately tied to systemic factors, such as poverty, discrimination, unemployment, and chronic health conditions. The authors’ review elucidates the negative impact of food insecurity on cancer treatment outcomes, and highlights the need for holistic interventions, including on-site, community, and federal initiatives. Addressing food insecurity within cancer care requires comprehensive, multilevel collaborations to improve nutritional status and health outcomes for patients with cancer. Despite growing awareness of food insecurity among patients with cancer, significant gaps remain in intervention development, access, and effectiveness. Existing clinical trials are limited, underscoring a lack of understanding of food insecurity’s impact on cancer care. Within cancer care, we need improved food insecurity screening, more collaborations across sectors, and rigorous research to evaluate intervention impacts. These steps, while potentially lacking immediate impact, are essential for sustainable health improvement and long-term food insecurity reduction. The intricate link between food insecurity and adverse cancer outcomes calls for comprehensive strategies, going beyond food provision, to address systemic issues of racism and poverty.
Key Points
1. The intersection of food insecurity and cancer: Patients with cancer face extensive medical demands that overshadow the vital role of nutrition in cancer care. Food insecurity, defined as inconsistent access to nutritious food, is a health-related social and medical need. Racial and ethnic minoritised groups, and other populations with limited socioeconomic status, are far more likely to be impacted by food insecurity during cancer care, and worse cancer outcomes.2. Financial toxicity exacerbates nutritional challenges: The economic implications of a cancer diagnosis are profound. Beyond medical bills, many face reduced income, leading to significant financial hardships. Such constraints amplify food insecurity, with patients resorting to cheaper, low-nutrient foods, which negatively impact their treatment outcomes, and heightens the risk of complications.
3. Multilevel solutions: The solution is not just to provide food access, but rather understanding and addressing the deeper social and economic determinants of health that underlie food inse-curity. Successful interventions demand collaborations across sectors, and a focus on both im-mediate relief and long-term systemic changes that promote equity. Early identification of food and nutrition insecurity in patients with cancer is crucial for impactful interventions, and im-proved outcomes.
INTRODUCTION
Cancer is an imposing condition that impacts individuals and their loved ones in multiple ways. Over the past 250 years, extensive research has begun to unravel cancer’s biological and organic causes.1 While there have been some critical milestones in cancer research, the focus on merely biological perspectives has inadvertently overlooked a crucial component of cancer care: addressing the multiple needs of patients that extend beyond medical treatment. This paper underscores one such overlooked aspect: the role and implications of food insecurity on cancer care.
When diagnosed with cancer, individuals often experience various physical and emotional changes that can be overwhelming, and difficult to navigate.2 Whether coping with the side effects of treatment,3,4 managing stress and anxiety,5 or financial toxicity,6 facing cancer can be an intimidating experience. Amidst this overwhelming state of medical demands and complicated and intensive cancer treatments, nutrition tends to be sidelined.7 However, nutrition is not a secondary concern, but a fundamental piece of cancer care.8 In this context, the intersecting issue of food insecurity becomes crucial to cancer care. A structured overview of the intersection between food insecurity and cancer care is depicted in Figure 1.
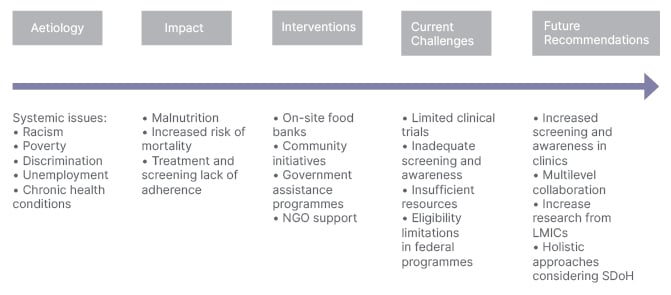
Figure 1: A structured overview of the intersection between food insecurity and cancer care.
LMIC: low- and middle-income countries; NGO: non-governmental organisation; SDoH: social determinants of health.
Food insecurity is the lack of consistent access to safe, nutritious, and adequate food to maintain an active and healthy lifestyle.9 The contributions to food insecurity cannot be attributed to one factor alone, but rather systemic issues, including poverty, discrimination, unemployment, and chronic health conditions.10-12 The prevalence and impact of food insecurity are far from uniform, varying based on sociodemographic characteristics, with some groups disproportionately affected, including individuals who self-identify as Black and Hispanic, and who are from low-income households.13 These disparities are often the result of broader systemic issues, such as poverty and the social determinants of health.14 Such patterns are interconnected with historical and systemic biases, which influence economic opportunities and outcomes over time.15
Food insecurity presents a major barrier to optimal receipt of cancer care. Studies estimate that up to 55% of patients with cancer experience food insecurity.16 This issue becomes more pronounced in low-income and medically underserved patients with cancer.17 Research conducted in Iran revealed that nearly 80% of patients undergoing cancer treatment struggle with food insecurity, with half of all patients with cancer suffering from hidden hunger.18 Similarly, a study on children with cancer in South Africa reported that 30% of these children were at high risk of poverty, highlighting a correlation between food insecurity and malnutrition, which subsequently negatively impacted their treatment outcomes.19 Despite the increasing evidence of the importance of nutrition among patients with cancer, a staggering 10–20% are estimated to die from nutrition-related issues.20
This review contains the latest research on how food insecurity impacts patients with cancer, the significance of addressing this issue in cancer care, and interventions to combat this growing problem.
IMPACT OF FOOD INSECURITY ON NUTRITIONAL STATUS AND TREATMENT OUTCOMES
Maintaining a healthy and well-balanced diet that includes sufficient proteins, vitamins, and minerals is essential for humans to reach optimal energy levels, and reduce the risk of developing chronic diseases or infections.21 For patients with cancer, a healthy diet is critical for optimal outcomes.8 This section will highlight the existing nutritional challenges patients with cancer experience, and the burden of food insecurity.
Cancer-related malnutrition, present in around 75% of patients with cancer,22 significantly contributes to multiple adverse treatment-related outcomes, and accounts for up to 20%20 of all cancer deaths. Cancer and its associated treatments introduce multiple nutritional challenges, including alterations in taste, gastrointestinal challenges, and psychological or psychosocial strain, impacting a patient’s appetite, and their ability to digest food effectively. Consequently, many patients with cancer may not be able to consume a sufficient quantity of healthy and necessary foods, which can lead to malnutrition, loss of muscle and bone mass, and decreased functional status.23
Malnutrition can have several consequences, including extended hospital stays, increased treatment-related toxicity, reduced health-related quality of life, and mortality.24-26 Furthermore, the nutritional status of a patient with cancer also plays a role in increasing the tolerability and effectiveness of some anti-cancer drugs.8
Due to the multiple nutritional challenges patients with cancer face, food serves as more than just fuel for the body. Unfortunately, these dietary demands are further intensified when patients with cancer experience an additional burden of food insecurity. The economic implications of a cancer diagnosis are profound. Not only do patients experience significantly expensive medical bills, but many experience loss of income after the diagnosis, due to the inability to work, or the need for assistance from a caregiver.27 Patients and their families struggling with financial toxicity are often forced to choose between meeting vital needs, such as rent, childcare, medications, nutritious food, and/or transportation. Such economic limitations further amplify food insecurity, as household finances become concerning to manage when expenses increase, income decreases, and priorities shift. Consequently, patients with cancer who experience food insecurity consume lower cost foods, which are less varied, poorer quality, and are lacking in essential nutrients, such as from vegetables, fruits, and dairy. This further worsens cancer-related malnutrition, and increases susceptibility to treatment complications.28
Correlations are prevalent between the populations burdened by cancer and those experiencing food insecurity. Socioeconomic status, race and ethnicity, cultural barriers, and educational attainment influence the prevalence and impact of food insecurity in patients with cancer.29 For example, low-income, immigrant, and minority populations with cancer experience elevated risk for financial hardship and food insecurity.17 Such elevated risk among these populations remains prevalent among patients who have completed treatment. For example, cancer survivors who are Black, Hispanic, or Latinx are twice as likely to experience food insecurity than cancer survivors who are White.30,31
Food insecurity also directly impacts patients’ ability to adhere to recommended treatment, and ultimately impacts cancer outcomes. For example, persistently food-insecure survivors of cancer are significantly more prone to skip medications and cancer-related treatment.32 Moreover, food insecurity among patients with cancer has been shown to impact adherence to colon, breast, and prostate cancer screening, as compared to patients without food insecurity.33,34
Patients with cancer who experience food insecurity also face a higher risk of mortality. This risk increases based on the severity of food insecurity, and any non-medical financial worries they may also experience. For example, patients with moderate and severe food insecurity are 53–69% more susceptible to mortality.35,36 Similarly, high levels of food insecurity are associated with greater incidence and mortality from cancer, specifically lung and colorectal cancer.37 A recent study among patients with gastrointestinal cancer with food insecurity showed 22% greater overall mortality among those with food insecurity than those without.38
Given the impact of food insecurity on patients with cancer, exploration of exacerbating barriers that may impede cancer care is crucial; for example, the lack of vehicle ownership restricts their ability to travel to areas with better food access.39 This situation is linked with the concept of food deserts, which are areas that have limited access to nutritious food due to socioeconomic and geographic limitations to food access.39 A recent study, which analysed how transportation barriers affect survivors of cancer, found that patients with cancer who faced such barriers were also three-times more likely to suffer from food insecurity than their counterparts, and to experience greater delays in their cancer care compared to those without transportation barriers.40 Such intersectional needs are important to address holistically, given that they are often co-occurring, and exacerbate the impact of food insecurity.
In essence, the additional burden that food insecurity poses on patients with cancer and their clinical outcomes is significant, particularly among minority populations, and those with socioeconomic disadvantages.19,41
APPROACHES TO MITIGATE FOOD INSECURITY IN CANCER CARE
Addressing food insecurity requires comprehensive and extensive multilevel collaborations to successfully mitigate the impact. Targeted interventions are essential for improving nutritional status and treatment outcomes among patients with cancer. These interventions can be broadly categorised into on-site (at the clinic), community, and federal programmes. Yet, gaps remain in understanding the feasibility, accessibility, and effectiveness of such programmes among patients with cancer. In low- and middle-income countries, non-governmental organisations play a significant role in financing and providing healthcare services, including food and financial support, to patients with cancer. These interventions provide ease of access, particularly in socioculturally diverse areas that are often fraught with economic and social barriers to high quality medical care.42
On-Site Programmes
On-site programmes that provide patients with food at the clinic where they receive care is one approach to improving food insecurity. Food banks and food pantries can assist in obtaining food, and distributing food to patients with food insecurity, in the clinic setting. Such options are especially important for patients who may be at risk of treatment delay, or who may forego treatment due to cost.43 Food banks and food pantries are often non-profit groups that gather food from various sources, such as grocery stores and restaurants with extensive storage facilities, and distribute it to the community, or directly to individuals in need.44 Clinic- and hospital-based pantries have a positive impact on patient-reported wellbeing, with patients reporting comfort and satisfaction with food options. These clinic- and hospital-based programmes have resulted in increased consumption of food and vegetables among patients overall.45 Other programmes, such as Feed1st, expanded distribution during the COVID-19 pandemic by eliminating identification or other restrictions to food access for patients, hospital visitors, and staff. Such programmes have resulted in increased distribution by maximising open access to food, and thereby removing the stigma.46
To date, many of these on-site programmes have not been specifically tailored to patients with cancer, but rather for patients generally in the primary care setting.43 The few examples of cancer-tailored, on-site food pantries include Food to Overcome Outcome Disparities (FOOD) in New York, USA,43 and the Legacy of Hope initiative in Philadelphia, Pennsylvania, USA.47 The FOOD programme tailors its services to the needs of patients with cancer by providing healthy meals that are low in sodium and sugar. Beyond merely providing food, it further offers bilingual (English and Spanish) nutritional education programmes for these patients. Moreover, the programme also provides a unique training course for healthcare providers, differentiating it from traditional food banks that primarily focus on broad food distribution.43
Limitations of on-site programmes apply to food pantries in general, in which the food may not alleviate all aspects of food security, such as providing a balanced diet, or meeting high demand. In addition, these programmes are limited in availability, as they are only within, or linked to, specific clinical settings. Such clinic-based programmes are frequently limited by insufficient resources, such as inadequate staffing, insufficient training, and restricted operating hours. As a result, these on-site food pantries have yet to meet the food security needs of their communities.45 Moreover, food pantries rely heavily on donations, which limits the availability and quality of food, and are usually stocked with unhealthy items. They can also evoke stigma and embarrassment, especially when restrictions for access are imparted.48 Innovative programmes and policies are needed to optimise food access.
Community and Home-Based Programmes
Community programmes offer both informal and formal strategies to support those who are food insecure. Informal approaches include seeking support from friends and family, who may provide food or money to address food insecurity. On the other hand, formal systems are more structured, and typically involve food banks or pantries, as discussed above.49 These community programmes operate at a local level, employing community gardens, meal delivery services, and the distribution of food, or grocery gift cards. While local community food pantries rely on volunteers and donations to provide necessary food, and programmes for those in the community that are in need, they differ from the on-site food banks, where patients receive the food directly within the clinic, eliminating the need for an extra trip. The primary difference between these two approaches lies in their operational structure and target population. Community pantries focus on serving the broader community, while on-site food banks within clinics primarily serve the nutritional needs of patients who are already accessing healthcare services.
Home-based programmes vary, and include home-delivered tailored meals. These meals are fully prepared, nutritionally tailored, and generally healthy for individuals living with advanced and costly diet-sensitive illnesses. One study shows that such meals can prevent approximately 1.6 million hospitalisations, and save up to 13.6 billion USD in costs annually.50 One randomised controlled trial, which included patients with metastatic lung and non-colorectal gastrointestinal cancers, demonstrated improved nutrition, independence, and reduced fatigue.51
Community gardens are also another approach associated with improved health and wellbeing. These gardens are open spaces where community members can collectively cultivate plants or flowers. While the evidence supporting community gardens is limited,52 there are some studies showing associated cancer risk reduction,53 and increased intake of fruits and vegetables among people with cancer.54 To date, there are no studies that evaluate the impact of community gardens on food insecurity among patients with cancer, however.
Food or grocery vouchers are also important interventions, and are designed to support patients by providing additional funds for their food budget.49 This may include debit cards that patients receive, with a prespecified amount of money, which are specifically created for the programme. These programmes are associated with higher levels of fruit and vegetable consumption among patients with cancer than the national average.55 These are also shown to increase the amount of household budget spent on healthy food items, and reduce the amount that patients with cancer spend on sweetened beverages and unhealthy foods.55 In addition, food vouchers have been shown to increase treatment completion rate among underserved patients with cancer,56 which may indirectly lead to improved survival, and decreased recurrence risk.
Federal Nutrition Programmes
Various federal agencies run Federal Nutrition Programs (FNP), which aim to provide nutritious food to low-income individuals and their families, pregnant people, infants, and children. To date, the government of the USA has implemented 16 FNPs to help address the growing problem of food costs, and help to stretch food budgets.57 The Supplemental Nutrition Assistance Program (SNAP), operated by the U.S. Department of Agriculture, and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), are two of the largest federally-funded programmes that address food insecurity among low-income households.
The SNAP programme, formerly known as food stamps, is the largest FNP in the USA that helps with food costs among low-income families, including those with children, seniors, and people with disabilities. SNAP improves food access and reduces food insecurity by 30%,58,59 and is associated with decreased poverty among eligible low-income households, and improved health outcomes.49 To qualify for the programme, individuals must meet three requirements: a gross monthly household income that is below 130% of the poverty line, a net household income below the poverty line, and a household asset limit.60 Populations not meeting these criteria, and undocumented migrants, are not eligible for such programmes. In the state of California, such programmes were also ineligible for people who were receiving Supplemental Security Income (SSI) benefits, until policy changes in June 2019, which expanded the programme among these populations as well.61
The WIC programme is another federally-funded programme. WIC is a short-term federal grant intervention programme for states, which aims to provide supplemental foods, healthcare referrals, and nutrition education to low-income females who are pregnant and postpartum, infants, and children up to age 5 years, who are at nutritional risk. To qualify for the programmes, applicants must have an annual household income below 185% of the USA’s poverty income guidelines, or be enrolled in the Temporary Assistance for Needy Families (TANF), SNAP, or Medicaid.62 Unlike SNAP, undocumented migrants are eligible for WIC benefits. Such programmes are associated with improvements in health outcomes, including longer pregnancies, fewer premature births, lower incidence of moderately low and very low birthweight infants, fewer infant deaths, and a greater likelihood of receiving prenatal care.63,64
Although FNPs like SNAP and WIC provide assistance to low-income individuals and families, they may not provide the nutritional support that many patients with cancer may need, and often do not meet the needs of underserved, immigrant, and limited English-proficient populations.43 Specifically, among patients with cancer who received SNAP benefits, 70% remained food insecure, and stayed at significant risk for the negative-associated outcomes of food insecurity.65 Furthermore, these programmes do not comprehensively address food insecurity, as many patients with cancer may be above the income eligibility cutoff, or cannot meet other criteria, such as immigration status eligibility. Such deficits are important to recognise, as food insecurity is often concentrated in minority and immigrant populations. Thus, programmes aiming to address food insecurity should comprehensively address the needs of patients with cancer and their households, who are most at risk for burden.
CHALLENGES AND FUTURE DIRECTIONS
Over the past decade, there has been much more attention on the growing problem of food insecurity, and the unique nutritional requirements of patients with cancer.7 Yet, gaps remain regarding interventions and their feasibility, accessibility, and effectiveness, that can overcome this critical problem. Currently, there are 106 clinical trials registered in the International Clinical Trials Registry Platform (ICTRP) for the term “food insecurity,” and 125 in the National Clinical Trials (NCT) registry. Nonetheless, when searching for trials related to both food insecurity and cancer, the numbers significantly drop to four on the ICTRP, and two on the NCT registry.
Adolescents and young adults (AYA; 15–39 years), a subset of survivors of cancer, face distinctive challenges, which are less characterised. Although AYA populations are often grouped with either children or adults, AYA populations face quite distinct developmental, psychosocial, and pathophysiological differences.66 These include the long-term effects of anticancer treatments, such as cardiovascular and bone diseases, and altered taste perceptions, leading to nutritional deficiencies. Such populations need further research to understand and overcome their specific needs.
The limited number of intervention trials indicates the first major challenge: a gap in our understanding of food insecurity’s impact on cancer care, and how to best address it. Most of the existing literature on food insecurity in patients with cancer, and survivors of cancer, is based on observational studies that aim to describe its prevalence and risk factors.67 Although the existing evidence is valuable, this limited view of the problem, which is often focused on an individual’s immediate needs, and not on the broader social determinants that are the root causes of the problem, provides short-term relief, and perpetuates this growing issue.
Multiple challenges arise when addressing food insecurity, as the solutions often require multilevel interventions, ranging from immediate food assistance programs to broad policy interventions that aim at systemic change. Such broader interventions must involve and address the non-medical, social, and economic factors that influence health and outcomes.29 These include addressing community-wide conditions, addressing systemic racism, and addressing policies that can sustain interventions, rather than focusing on the immediate social needs of the individual, such as providing transportation, food, or housing. Given that emergency food resources only provide immediate relief for 29% of households in the USA which are suffering from food insecurity, interventions must address the root causes of food insecurity and poverty to eliminate this issue. Hence, systemic changes are required to ensure long-term solutions.43
Specifically, as related to patients with cancer, addressing food insecurity requires support throughout stages of treatment.16 First, awareness and screening of food insecurity is a fundamental first step in addressing this problem. To date, few oncology clinics have embedded Registered Dietitian Nutritionists, and even among those that do, few clinicians ask patients with cancer about their ability to afford or obtain food. This is despite the growing recognition that food insecurity can impact patient outcomes.68 Targeted education and training to improve the screening and management of food insecurity is the first step in addressing such problems. Programmes such as the World Cancer Research Fund (WCRF), the American Institute for Cancer Research (AICR), and the Continuous Update Project (CUP) offer key resources. The AICR provides tools for dietary needs and health, while the CUP shares updated research on nutrition’s impact on cancer. Second, collaborations across multilevels should engage patients, caregivers, clinicians, community-based organisations, patient advocacy groups, policymakers, and other researchers, to invest in the co-development of both immediate interventions and long-term systemic changes at a community level. While the impact of these efforts may not be immediately evident, they are essential to promoting sustainable health improvement, and reducing food insecurity in the long term.69 Finally, rigorous research to evaluate the impact of interventions on food insecurity among patients with cancer is needed to demonstrate the clinical benefit, and the return on investment to support policy implications. This research should entail more randomised controlled trials investigating the effectiveness, and should align household, community, and policy-level interventions to comprehensively tackle food insecurity.49
CONCLUSION
The complex and unexplored relationship between food insecurity and adverse cancer outcomes, particularly among low-income and minority populations, demands a multifaceted approach that extends beyond merely providing food to patients with cancer. Interventions must address the more profound social and economic causes, including systemic issues of racism and poverty. In high-income countries, collaborations between hospitals and on-site food distribution programmes could be enhanced, and widely adopted. In contrast, in low- and middle-income countries, where infrastructure and resources may be limited, non-governmental organisations can play a vital role by providing food aid and educational resources, and bridging the gap between patients and available government programmes. To mitigate food insecurity, comprehensive, multilevel collaborations encompassing patient and clinician education, broader policy interventions, and rigorous research are needed to ensure immediate relief, but with long-term, sustainable, and systemic changes. Incorporating screening for food and nutrition insecurity can significantly improve patient outcomes. Early identification of these health-related social needs will allow for timely interventions that can improve patient outcomes.







