Abstract
Introduction: Breast sensibility following reconstruction surgery, though often overlooked, holds significant importance due to its widespread occurrence and profound effects on patients’ well-being and safety. The author’s objective is to compare the sensory outcomes between deep inferior epigastric perforator (DIEP) flap microsurgery reconstruction and implant-based reconstruction. Additionally, the potential influence of sociodemographic and clinical factors on sensory recovery is explored, along with assessing temperature discrimination abilities and evaluating quality of life.
Material and methods: An ambispective descriptive-analytical study was conducted involving women who underwent mastectomy with reconstruction using either DIEP flap and implants at the author’s hospital between 1990–2021. Data were collected from medical records, patient histories, physical examinations, and validated quality of life questionnaires (BREAST-Q). Spearman’s or Pearson’s correlation coefficients were employed for the analysis of quantitative variables, while the Student’s T test or Mann-Whitney U test were used to compare quantitative and qualitative variables.
Results: A total of 99 women with breast reconstruction were included, 47 with DIEP flap and 52 with implants. Sensory recovery in implant-based reconstruction was found to be superior to DIEP flap reconstruction (5.03 and 5.18, respectively; p<0.005). A direct correlation was observed between sensory improvement and thermal discrimination (Spearman coefficient 0.9; p<0.001). Factors such as radiotherapy, delayed reconstruction with DIEP flap, and height with implants were associated with poorer sensory recovery in the breast. Women experiencing better breast sensibility reported higher satisfaction with their surgeon, medical team, and psychosocial quality of life.
Conclusion: Women reconstructed with implants or DIEP abdominal flap exhibit suboptimal overall sensory recovery of the reconstructed breast, with slightly better outcomes observed in women reconstructed with implants. The development of novel surgical techniques aimed at enhancing sensibility after breast reconstruction could significantly benefit these patients.
Key Points
1. The study compares sensory outcomes between deep inferior epigastric perforator flap and implant-based breast reconstruction, with implant-based reconstruction showing slightly better sensory recovery.2. The research provides valuable insight into the factors influencing sensory recovery, which can guide surgeons in making more informed decisions about the best reconstruction technique for each patient.
3. The findings emphasise the importance of considering both aesthetic and functional outcomes, aiming to enhance patient satisfaction and quality of life after breast reconstruction surgery.
INTRODUCTION
Breast cancer is the most common cancer worldwide, accounting for 12.5% of all new cancer cases per year.1 According to the Spanish Society of Medical Oncology (SEOM), 34,750 women were diagnosed with breast cancer in Spain in 2022.2 Furthermore, it is the leading cause of cancer-related death among Spanish women. Due to its significant prevalence and mortality, the modernisation of breast reconstruction techniques is necessary to offer better results and quality of life for those women.3
At the hospital where this study was conducted, the two main procedures performed were microsurgical reconstruction with the deep inferior epigastric perforator (DIEP) abdominal flap and reconstruction with implants.
Microsurgical breast reconstruction with DIEP involves taking an abdominal flap with its skin, fat, and blood vessels, and extracting it from the body for transplantation to the breast of the same patient.4,5 This technique was described by surgeon Koshima in 1989 and has been used since then, currently being one of the most popular techniques for breast reconstruction.6 Based on several clinical trials, the DIEP flap has proven to be a valuable reconstructive method for many women, with low complications and a significant satisfaction with the result, as it creates a natural appearance, identical touch, and consistency to the healthy breast. Unlike the transverse rectus abdominus myocutaneous (TRAM) flap, which uses muscle, the DIEP flap spares muscle, resulting in shorter recovery times and fewer complications, such as hernias.7-9 Therefore, nowadays reconstruction with the DIEP abdominal flap is preferred.10,11 Furthermore, innervation to the flap is increasingly being included in DIEP surgical procedures to improve sensory recovery in that area. Research using sensory segments of the intercostal nerve has shown promising results, as it has been demonstrated that sensory recovery in innervated flaps is superior and develops earlier compared to non-innervated flaps.12,13 Another study has confirmed improved breast sensibility with innervated flaps, as well as a higher physical well-being with breast appearance in the BREAST-Q questionnaire.14
Reconstruction using implants is a breast reconstruction alternative, which was first described in the 1960s and is realised by placing a submuscular implant below the pectoralis major muscle. At the author’s hospital, reconstruction with an expander is used initially to allow breast tissue expansion. The expander, equipped with a valve for fluid inflation, is gradually enlarged over several months until the desired breast size is reached, followed by a second surgery to insert the permanent implant.15 The main drawbacks are the requirement of two-stage surgery and the less natural result. However, the main complication is capsular contracture, which is the formation of fibrotic scar tissue around the implant, resulting in hardness, discomfort, and pain in the breast area. This complication is often associated with radiotherapy, making implant-based reconstruction unsuitable. Radiotherapy thins the skin, limits breast projection, hampers healing, and can cause implant perforation or extrusion.16,17
Both reconstruction techniques can be performed simultaneously with mastectomy or in a second-stage surgery. Delayed reconstruction allows histopathological analysis of the tumour and accomplishment of oncological treatment before reconstruction.18 Both techniques are valid, but studies have shown better recovery and fewer complications in patients undergoing two-stage reconstruction, although it is always necessary to evaluate each patient’s individual preference. However, immediate breast reconstruction is increasingly performed because several studies have not shown a higher risk of complications or worse patient satisfaction with breast appearance.18-20
Regarding breast sensibility, it is a poorly investigated matter because research has prioritised achieving better aesthetic and long-lasting results after surgery.21,22 However, it is important to assess breast sensibility, as it has an impact on women’s intimate life, and having good sensibility prevents injuries, such as traumas or burns. Sensibility is measured by the cutaneous pressure threshold in nine areas of the breast using Semmes-Weinstein monofilaments, being held in each area for approximately 1.5 seconds. The measurement takes place in a consultation room with appropriate temperature and humidity, with the patient lying down, the breast exposed, and their eyes closed.23,24 Therefore, measuring the degree of breast sensory recovery with these two techniques will allow data and conclusions to be established to better understand which factors influence breast sensibility and compare which procedure offers greater sensory recovery. This study will help apply these results in surgical procedures or future research, to improve the quality of life of women who are breast cancer survivors.25
MATERIAL AND METHODS
Objectives
Main objective
To compare the level of breast sensibility with microsurgical reconstruction and implant reconstruction in women undergoing breast reconstruction with DIEP and implants at the Plastic Surgery Department of the author’s hospital from 1990–2021.
Secondary objectives
- To compare thermal discrimination to heat and cold between DIEP reconstruction and breast implant reconstruction.
- To assess the aesthetic and sensory satisfaction of patients using the Breast-Q questionnaire, thereby evaluating their quality of life and postoperative satisfaction.
- To determine whether previous neuropathies, cardiovascular risk factors (such as diabetes or smoking), weight, or age influence sensibility.
- To investigate differences in sensory recovery among women who have received chemotherapy, radiotherapy, or hormonotherapy, and whether it was administrated in a neoadjuvant or adjuvant setting.
- To compare differences in sensory recovery between immediate and delayed breast reconstruction.
Study Population
A study involving 99 women who underwent breast reconstruction surgery at the Plastic Surgery Department of the University Hospital of Getafe from 1990–2021 was conducted. The procedures included microsurgical reconstruction with the DIEP flap and reconstruction with implants.
Inclusion criteria
All women aged 18 years and above who underwent primary breast reconstruction with implants or DIEP following breast cancer mastectomy.
Exclusion criteria
Women who underwent mastectomy of the contralateral breast were excluded from the study. Additionally, women who experienced any complications or implant/flap rejection resulting in its removal were excluded. Those who later experienced tumour recurrence were also excluded.
Data Collection
Each patient was selected from a database provided by the Plastic Surgery Department at the University Hospital of Getafe, Madrid, Spain, ensuring adherence to the inclusion and exclusion criteria. Their medical records were accessed to gather comprehensive information regarding their intervention, surgical procedure, recovery, oncological treatment, and medical history. Subsequently, selected patients were scheduled for a consultation to perform sensibility measurement, thermal discrimination test, medical history review, and physical examination. To avoid biases, appropriate temperature and humidity levels were maintained in the consultation room.
For quantifying breast sensibility, Semmes-Weinstein monofilaments were utilised. These nylon filaments facilitate the assessment of tactile sensibility in specific areas. The filaments bend under applied pressure, maintaining a constant pressure of typically 10 g regardless of the force exerted by the examiner. Different types of monofilaments, identified by numbers ranging from 1.65–6.65, were used, with higher values indicating larger diameters and poorer skin sensibility in the area being studied.
The breast was divided into nine different points, starting from the nipple areola.
Semmes-Weinstein monofilaments were applied to each point on both breasts, while patients lay on the consultation bed with their eyes closed.12 Patients were asked to indicate whether they felt each monofilament, and the smallest monofilament with which skin sensibility was perceived was recorded for each area. Following the sensory examination, a thermal discrimination test was conducted using bottles of physiological saline heated to 60 °C and cooled to 4 °C, assessing the ability to discriminate temperature at the nine points of both breasts.
After the sensory and thermal examinations, patients were given the BREAST-Q questionnaire, enabling evaluation of satisfaction levels across various aspects of the breast reconstruction process. This questionnaire addressed satisfaction with the breast, overall outcome, quality of care received, and quality of life (including physical, psychological, and sexual well-being of the patient).
Statistical Analysis
In the descriptive analysis, qualitative data were presented as relative frequencies (n) and absolute percentages (%). For quantitative variables, the team first verified normal distribution using the Shapiro-Wilk test. If the variables exhibited normal distribution, they computed the mean and standard deviation. Alternatively, if the normal distribution was not observed, they reported the median and interquartile range.
In the bivariate analysis, various tests were employed to evaluate the relationship between breast sensibility and potential influencing factors. Specifically, for analysing the association of quantitative variables, the team utilised Pearson correlation when normal distribution was met and Spearman correlation otherwise. To examine the association between a quantitative variable and a dichotomous qualitative variable, they employed Student’s t-test for independent samples under normality assumptions, or the Mann-Whitney U test otherwise. In cases where the qualitative variable was polytomous, ANOVA for independent samples was applied if the variables followed a normal distribution, while the Kruskal-Wallis test was used if not.
A p-value <0.05 was considered statistically significant.
RESULTS
Population Description
Between 1990–2021, the team identified 877 mastectomised patients who had undergone breast reconstruction at the hospital. Among them, 103 underwent reconstruction with DIEP flap and 774 underwent reconstruction with implants.
Of the 103 patients who underwent DIEP abdominal flap reconstruction between 2005–2020, all met the inclusion criteria, but some were excluded for the following reasons: two due to death, 20 because they did not want to participate in the study, and 34 due to lack of time and availability.
Of the 774 patients who underwent prosthetic reconstruction, 88 were excluded due to death, 85 because they did not want to participate in the study, and 174 due to lack of time and availability. Another 427 patients were excluded due to lack of data and or not meeting the criteria due to the following reasons: having subsequent reconstructions with other surgical techniques (DIEP, TRAM), removal of the prosthesis, or having undergone bilateral mastectomy. Ultimately, the sample consisted of 47 patients with DIEP reconstruction and 52 patients with implant reconstruction, being the sample with both types of reconstruction, 99 patients.
Out of the 99 women included in the study, the age range was 38–82 years old, with a significant age gap between the two reconstruction techniques, indicating that women with implants were, on average, 13.7 years older.
Regarding the clinical history of the studied patients, the pack years index had a higher median in women reconstructed with DIEP flap (11.3) compared to those with implants (8.97). Similarly, the relative frequency of smokers was higher among women reconstructed with DIEP flap compared to those with implants (19.1% and 9.6%, respectively). Moreover, the relative frequency of smokers during the reconstruction process, spanning from reconstructive surgery to the following 18 months, was slightly higher in women reconstructed with DIEP flap.
There were notable differences in the oncologic treatment received between both reconstructions. While tumour resection prior to mastectomy was common overall (25.3%), it was slightly more prevalent in women with implants than in those with DIEP flap (28.8% versus 21.3%, respectively). However, women reconstructed with DIEP flap received more chemotherapy, immunotherapy, and hormonotherapy than those with implants. In both types of reconstructions, chemotherapy and radiotherapy were administrated adjuvant rather than neoadjuvant. Additionally, there were mostly no postoperative complications, with touch-ups being the most frequent complication.
The surgeries performed on the contralateral breast differed significantly between the two reconstruction techniques. For instance, most women with flap reconstruction did not undergo any intervention on the other breast (38.3%), and among those who did, breast reduction was the most common procedure (31.9%), followed by mastopexy (25.5%). Conversely, among women with implant reconstruction, the vast majority underwent mastopexy on the contralateral breast (65.4%), followed by breast reduction (21.2%).
In the study, patients who underwent implant-based reconstruction had been reconstructed for a longer period than those reconstructed with DIEP flap, with a statistically significant difference of 8.87 years.
Comparison Of Breast Sensibility
Breast skin sensibility is better with lower Semmes-Weinstein monofilament values depicted in the graphs. Reference values are based on measurements from areas 1–4 and 5–9, which are 4.54±1.16 and 5.69±0.93 with DIEP compared to 4.48±0.97 and 5.47±0.80 with implants, respectively. Consequently, skin sensibility is slightly higher in breasts reconstructed with implants than in those reconstructed with DIEP. The effect size (Cohen’s d) for this difference is 0.18, indicating a small effect. The difference in skin sensibility between DIEP and implant can be observed visually in Figure 1, where a positive difference indicates higher sensibility with abdominal flap compared to implants, suggesting poorer sensibility with DIEP.
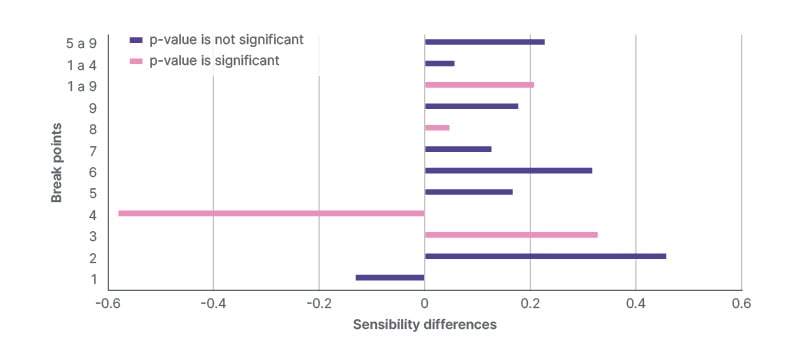
Figure 1: Sensibility differences between deep inferior epigastric perforator and implant reconstructions across nine points.
P value of the paired samples T-test.
The sensibility differences illustrate the reduced sensibility of the reconstructed breast in comparison to the healthy one (Figure 2). Across most points (excluding 1 and 4), differences are more significant with DIEP than with implants, signifying better sensitivity recovery with implant-based reconstruction.
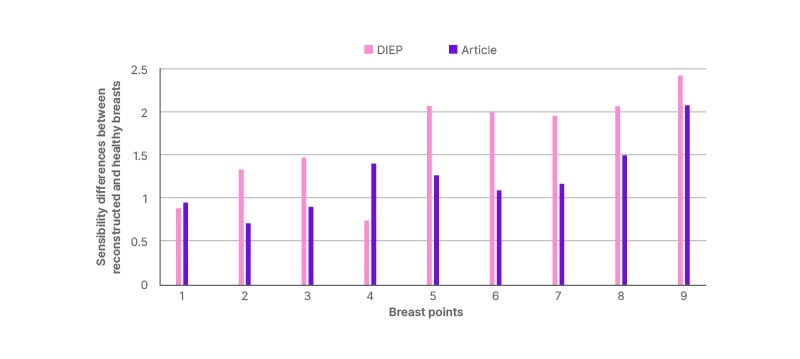
Figure 2: Sensibility differences between reconstructed and healthy breasts with deep inferior epigastric perforator and implants.
P value of the paired samples T-test (p<0.001).
DIEP: deep inferior epigastric perforator.
Thermal Discrimination Ability
Regarding heat sensitivity, breast reconstructions with implants demonstrate superior responsiveness to hot temperatures in seven of the evaluated areas compared to those with DIEP. Additionally, across both reconstruction methods, the capacity to detect heat is notably higher in areas 1–4 compared to areas 5–9, with frequencies falling below 30% in the latter. For cold sensitivity, eight out of the nine studied areas exhibit better responsiveness to cold temperatures in implant-based reconstruction compared to DIEP flap reconstruction. Similarly, it is observed that in both reconstruction techniques, the ability to detect cold is notably higher in areas 1–4 than in areas 5–9. However, it is worth mentioning that frequencies in detecting cold in areas 5–9 are relatively higher in implant reconstruction.
The correlation between the mean breast sensibility and thermal discrimination with each reconstruction technique in the nine points was assessed using Pearson’s rank correlation. Statistically significant associations were found for both reconstruction techniques. Thus, a lower mean sensibility calculated with monofilaments corresponded to a greater heat and cold sensibility.
BREAST-Q Questionnaire
The Breast-Q questionnaire assesses satisfaction levels across various aspects of the reconstruction process, with a higher score indicating greater personal satisfaction with each scale. In both reconstruction techniques, scores are consistently above 50% across all scales, except for physical well-being with the postoperative chest in both reconstructions and satisfaction with the effects of radiation in microsurgical reconstruction.
To compare DIEP and implant reconstructions, the score difference is calculated for scales present in both BREAST-Q questionnaires. The satisfaction scores for breasts in the preoperative period, and with information and surgeon, are higher in DIEP reconstruction than in implant-based reconstruction (p<0.005). The effect sizes (Cohen’s d) for these differences are 0.62 for preoperative breast satisfaction, 0.58 for satisfaction with information, and 0.55 for satisfaction with the surgeon, indicating medium effects.
The correlation between BREAST-Q questionnaire scores and sensibility was statistically analysed for each breast reconstruction. Higher breast sensibility with implant-based reconstruction corresponds to higher scores in satisfaction with their breasts preoperatively, satisfaction with the surgeon, and satisfaction with the medical team (p<0.005).
Sensibility and Sociodemographic-Clinical Variables
The association between breast sensibility and the studied sociodemographic and clinical variables is observed in Table 1. In implant-based reconstruction, a statistically significant yet mild correlation is found between sensibility and height (r=-0.36; p=0.008), indicating that higher height corresponds to lower monofilament values and therefore better cutaneous sensibility. This represents a medium effect size (Table 1).
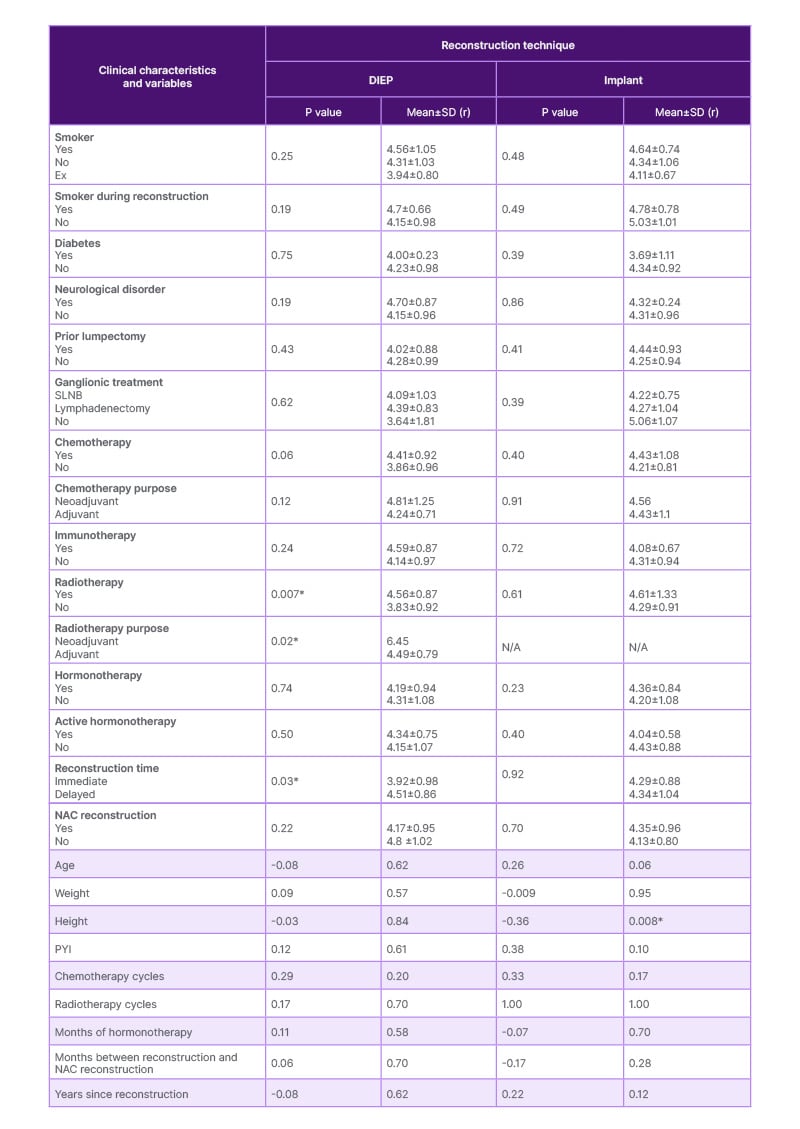
Table 1: Bivariate analysis of the correlation between sensibility and qualitative and quantitative variables for each type of reconstruction.
P value for dichotomous variables with Student’s t-test or Mann-Whitney U test and for non-dichotomous variables with ANOVA or Kruskal-Wallis test.
*P value is stastically significant (<0.05).
BMI: body mass index; DIEP: deep inferior epigastric perforator; NAC: nipple-areola complex; PYI : pack years index; r: Spearman’s correlation coefficient; SLNB: sentinel lymph node biopsy.
In DIEP flap reconstruction, statistically significant differences are noted between sensibility and radiotherapy (p=0.007), indicating worse sensibility in women treated with radiotherapy. The effect size (Cohen’s d) for this difference is 0.82, representing a large effect. Additionally, better breast sensibility is associated with adjuvant radiotherapy received after reconstruction rather than neoadjuvant (p<0.005). Furthermore, statistically significant differences are observed regarding the timing of reconstruction in relation to mastectomy (p=0.03), revealing worse breast sensibility when reconstruction is delayed. The effect size (Cohen’s d) for this difference is 0.64, indicating a medium effect (Table 1).
DISCUSSION
The aim of this study was to compare breast sensibility between the two most prevalent breast reconstruction methods: DIEP flap and breast implants. Generally, sensibility with implants is superior due to minimal skin modifications during reconstruction. Conversely, with DIEP microsurgical reconstruction, transplanted autologous abdominal skin tissue may lead to insensitivity in the breast area due to skin modifications.
However, the difference in breast sensibility between the two techniques was smaller than expected.22 The mean sensibility measured at points 1–9 was 5.03±1.01 with implants and 5.18±1.18 with DIEP, varying by only 0.21 monofilament units. This slight difference may be attributed to insensitivity caused by radical mastectomy, irrespective of the reconstruction method employed.
Breast sensibility is generally better with implants, except at points 1 and 4, where DIEP reconstruction exhibits higher sensitivity. These two points correspond to the upper quadrant of the breast, where the skin is preserved during the DIEP flap reconstruction process. Plus, a significant loss of sensibility in flap skin leads to higher sensibility with implants at points 5–9.
Secondary objectives focused on evaluating thermal discrimination capacity, patient satisfaction with the reconstruction process, and other clinical and sociodemographic factors potentially related to sensibility. In the thermal discrimination test, the ability to discern cold and heat was generally better in implant-based reconstruction, except at point 4, possibly due to the presence of healthy skin in DIEP reconstruction at this point. However, both reconstructions exhibited difficulty in determining heat at points 5–9, increasing susceptibility to accidental burns. Higher scores on the Breast-Q questionnaire were found in satisfaction with the surgeon, the medical team, and other staff, as well as in psychosocial well-being. Women with DIEP reconstruction reported greater satisfaction with the information and with their breasts preoperatively compared to those with implants. Additionally, higher breast sensibility correlated with increased satisfaction with the surgeon and medical team in women with implants.
Although the BREAST-Q scores provided useful insights into patient satisfaction, a deeper analysis of the qualitative feedback would enrich the understanding of its impact on quality of life. Some patients were unable to respond to open-ended questions due to time constraints, and while others provided detailed feedback, this qualitative data has not yet been fully analysed. However, during clinical examinations, patients frequently expressed high satisfaction with their care, which underscores the importance of examining this qualitative feedback in future studies for a more comprehensive view of patient experience.
Limitations of the study include a lack of research comparing breast sensibility between microsurgical reconstruction and implants, constraining comprehensive literature review, and results comparison. Time constraints also affected data collection, as being a prospective study, scheduling with patients depends on availability, leading to potential biases in patient selection.
One of the critical limitations of this study was the time bias between the two groups, where women who underwent implant-based reconstruction had their surgeries, on average, nearly a decade earlier than those who received DIEP flaps. This difference in time since surgery is a significant factor when considering sensory recovery outcomes, as multiple studies have shown that sensory recovery after breast reconstruction improves gradually over time. Since the implant group had significantly more time to heal, their sensory recovery may appear better simply because they have had more time for sensory reinnervation and adaptation. In contrast, women in the DIEP group, with less time since surgery, might still be in earlier phases of sensory recovery, leading to a lower measured sensitivity at the time of assessment. This temporal discrepancy could confound the results, making it difficult to attribute the differences in sensory recovery solely to the reconstruction technique. Women who underwent implant reconstruction may have benefited from having more post-surgery years, giving nerves more time to regenerate, whereas the sensory outcomes for the DIEP group might improve further with additional follow-up time.26 Thus, the study’s finding that implant-based reconstruction results in superior sensory recovery should be interpreted with caution, as it may partially reflect this difference in recovery timelines rather than a true advantage of one technique over the other. To mitigate this bias in future research, controlling for time since surgery in statistical analyses could provide a more accurate comparison of sensory outcomes between the two groups.
The role of radiotherapy in influencing breast sensibility outcomes is nuanced, with several factors playing a key role. This study highlighted that timing, particularly the distinction between neoadjuvant and adjuvant radiotherapy, has a significant impact on sensory recovery. Women who received adjuvant radiotherapy demonstrated better sensory outcomes compared to those who received it in a neoadjuvant setting. This suggests that delaying radiotherapy until after reconstruction may allow for improved nerve regeneration or reduce the adverse effects of radiation on the healing process.27,28 However, while timing appears to be a critical factor, this study is limited in its exploration of specific radiotherapy dosage and cycle variations. These variables could also influence sensory recovery but were not extensively examined in this dataset. Future research with a more detailed focus on the radiotherapy regimen, including dosage and the number of cycles, would be necessary to fully understand their relationship with breast sensibility.
In addition to sensibility outcomes, it’s important to consider other factors that influence the choice between DIEP flap and implant-based reconstructions. Cost-effectiveness analysis shows that while DIEP flap procedures have higher initial costs due to longer operating times and hospital stays, they may be more cost-effective in the long term due to fewer complications and revision surgeries compared to implant-based reconstructions.29 Recovery times also differ significantly; patients undergoing DIEP flap reconstruction typically require a hospital stay of 3–5 days and 4–6 weeks before returning to normal activities, whereas implant-based reconstruction patients often have shorter hospital stays of 1–2 days and can resume normal activities within 2–4 weeks.30 However, implant-based reconstructions may require more frequent follow-up visits and potential revision surgeries over time due to complications such as capsular contracture or implant rupture.31,32 These factors should be carefully considered alongside sensibility outcomes when deciding between reconstruction techniques.
CONCLUSION
Breast sensibility at points 1–4 in women reconstructed with implants averaged 4.48±0.97, while in women with DIEP it averaged 4.54±1.16, indicating a minimal difference of 0.06 monofilament units. At points 5–9, sensibility with implant-based reconstruction averaged 5.47±0.8, compared to 5.69±0.93 with microsurgical reconstruction, showing a difference of 0.23 monofilament units. Overall, sensitivity recovery was slightly better in implant-based reconstruction, although sensibility is higher with DIEP than with implants at point 4. Moreover, sensibility was constantly better at points 1–4 than at points 5–9 of the breast. The difference between DIEP and implant reconstruction across all points of the breast (1–9) was 0.21 units, indicating superior sensibility in breasts reconstructed with implants.
The capacity for thermal discrimination, both for heat and cold is generally better in implant reconstruction compared to DIEP reconstruction, except at point 4. Thermal discrimination with implant-based reconstruction constantly exceeded 50% for points 1–4. In both breast reconstruction techniques, the inability to discriminate thermal stimuli is associated with poorer skin sensibility.
In DIEP microsurgical reconstruction, treatment with radiotherapy is associated with decreased breast sensibility, and adjuvant radiotherapy is linked to better sensibility compared to neoadjuvant therapy. Additionally, women undergoing delayed reconstruction have poorer sensibility than those with immediate reconstruction post-mastectomy. In implant reconstruction, increased sensibility is associated with greater patient height. However, the number and duration of oncological treatments do not seem to influence breast sensibility in either reconstruction method.
Regarding the BREAST-Q questionnaire, most scale scores exceed 50%, indicating high satisfaction levels, particularly in psychosocial well-being. However, scores were lower than 50% in physical well-being with the postoperative chest and in adverse effects of radiotherapy. In implant-based reconstruction, higher sensibility values are correlated with greater satisfaction with breasts preoperatively, the surgeon, and the medical team.
This study provided valuable insights into breast reconstruction techniques, comparing sensory recovery between DIEP flap and implant-based methods. While implant-based reconstruction showed slightly better overall sensory recovery, DIEP flap offered long-term cost-effectiveness and fewer complications. Importantly, this research can aid in patient care and decision-making, guiding personalised reconstruction choices based on individual needs. Furthermore, as microsurgical techniques continue to evolve, the potential of innervated flaps presents a promising avenue for improving sensory recovery, which could significantly enhance patient outcomes. Future studies should focus on this emerging area to further refine breast reconstruction techniques.
ETHICAL STATEMENT
The research study was approved by the Committee of Ethics in Drug Research (CEIm) of the University Hospital of Getafe on 30 January 2023. The research study was conducted in accordance with bioethics regulations following the Helsinki Declaration, the Belmont Report; the Oviedo Convention on Human Rights and Biomedicine; and Law 14/2007, of July 3, on biomedical research. It also complied with EU legislation on personal data, specifically Organic Law 3/2018, of December 5, on the Protection of Personal Data and guarantee of digital rights, Royal Decree 1720/2007, Law 41/2002, of November 14, which regulates the basic rights of patients and obligations regarding information and clinical documentation. All study patients were identified by a case code in a database, through pseudonymisation of the initial database. Confidentiality of patients’ personal data was respected at all times, and data could not be copied or used for purposes other than those determined, nor transferred to other individuals not involved in the study.







