BACKGROUND AND AIMS
Targeted therapy and immunotherapy have revolutionised the treatment of metastatic non-small cell lung cancer, particularly adenocarcinoma.1 Among non-small cell lung cancer cases, around 8–10% are ALK-positive,2 with the majority involving EML4-ALK gene variants.3 This study aimed to explore the connection between ALK gene variants and programmed death-ligand 1 (PDL1) expression in patients with metastatic lung adenocarcinoma, focusing on relevant clinical parameters, as there is limited data from the Indian cohort on this subject.
MATERIALS AND METHODS
A retrospective analysis was conducted on data collected from 17 patients with advanced lung adenocarcinoma with ALK gene mutations. The anaplastic lymphoma kinase protein variants were determined through next-generation sequencing, while PDL1 expression was assessed using immunohistochemistry with the sP263 antibody. These findings were then correlated with relevant clinical parameters.
RESULTS
The median age of the patient cohort was 46 years (range: 28–65). Among 17 of the patients who were ALK-positive, the majority had EML4-ALK gene fusions, with V1 (47.05%), V3 (35.20%), and V2 (11.70%) being the most common variants. V1 was more prevalent in females (87.5%) than males (12.5%). PDL1 negativity was observed in 64.7% of patients, while 35.2% were PDL1-positive. Specifically, PDL1 negativity was more common in the V1 variant, whereas PDL1 positivity was associated with V3. Brain metastases were more frequent in the PDL1-negative cohort (35.2%), and bone metastases and malignant pleural effusions were more common in V1 compared with V2 and V3. ALK positivity was observed in various metastatic sites with varying frequencies (Table 1).
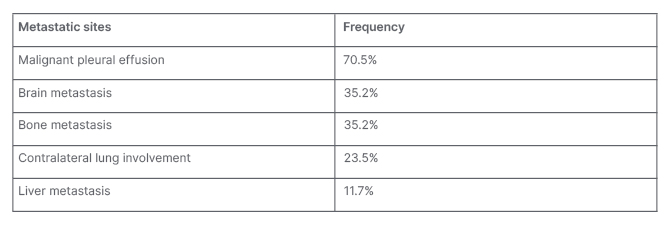
Table 1: Metastatic sites and their incidence for ALK-mutated non-small cell lung cancer.
CONCLUSION
The study concludes that V1 and V3 EML4-ALK gene variants are prevalent in patients with metastatic lung adenocarcinoma. It reveals a significant association between PDL1 expression and specific ALK variants, with V1 being more frequently associated with PDL1 negativity, and V3 with PDL1 positivity. Additionally, the V1 and V3 variants were more commonly found in female patients, and were associated with brain metastases and malignant pleural effusions. This real-world experience contributes valuable insights into treatment responses in this specific patient population.







