INTRODUCTION
Analyses on tumour-infiltrating lymphocytes (TIL) to date have mainly evaluated stromal TIL and possibly intratumoural TIL. The authors of this study were not able to find any analyses in which TIL were evaluated spatially, by stromal or intratumoural categories, separately by compartments of central tumour and invasive margin, nor any with prognostic values for the evaluation of this arising biomarker.
METHODS
The authors retrospectively analysed consecutive samples of 152 patients with early triple-negative breast cancer (TNBC) treated at an institution in Croatia from 2009–2012. TIL were assessed morphologically by haematoxylin and eosin stain using standard formalin-fixed paraffin-embedded samples according to the International TILs Working Group recommendation for the evaluation of TIL. Stromal TIL (sTIL) and intratumoural TIL (iTIL) were assessed spatially in compartments of central tumour (CT) and invasive margin (IM).1,2
RESULTS
Spatial analysis revealed that the most prevalent TIL were sTIL at IM, with median intensity of 30%, and as many as 85.5% of patients with intensity ≥10%. The rarest TIL and with lowest intensity were iTIL in CT, with a median intensity of 1.0% and only 23.0% of patients with ≥10% intensity. One-quarter of patients had TIL >50% in any of the evaluated compartments. There was a statistically significant correlation between sTIL and iTIL in the presence of TIL in all four evaluated compartments; the correlation was stronger among sTIL and iTIL in CT and sTIL and iTIL at IM, than between the two separate spatial compartments. In a bivariable analysis, all TIL indicators were statistically significantly associated with longer disease-free and overall survival. Patients with TIL ≥10% in all four evaluated compartments (sTIL and iTIL, in CT and IM) were shown to have statistically significantly less risk of disease recurrence or death, compared to those with TIL <10%. After adjustment for potential confounders using Cox proportional hazard regression, significant predictors of overall survival were sTIL (p=0.007), iTIL if present in ≥10% (p=0.022), IM TIL (p=0.002), sTIL at IM (p=0.001), and iTIL at IM if present in ≥10% (p=0.036).
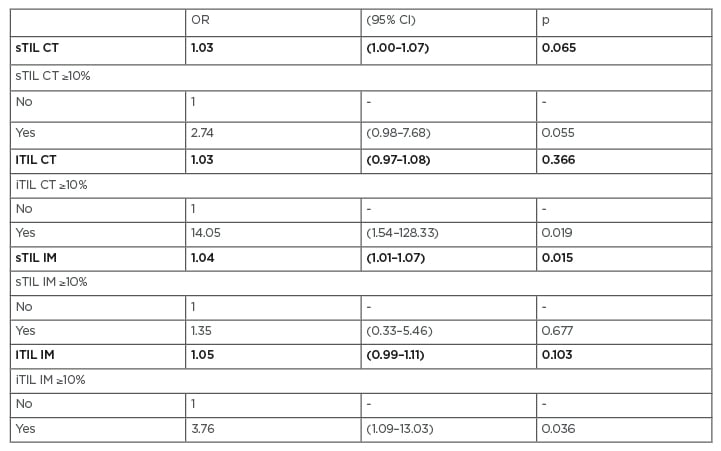
Table 1: Multivariable analysis of correlation of tumour-infiltrating lymphocytes and tumour-infiltrating lymphocytes ≥10% by compartments (stromal tumour-infiltrating lymphocytes and intratumoural tumour-infiltrating lymphocytes, in central tumour and at invasive margin) to 5-year overall survival (n=152).
Adjusted for age, comorbidities*, menopausal status, histology, tumour size, nodal involvement, stage, grade, Ki-67, surgery, and chemotherapy†.
*Data missing for six (3.9%) patients, supplied as if no comorbidities.
†Data missing for four (2.6%) patients, supplied as if no adjuvant chemotherapy.
CI: confidence interval; CT: central tumour; IM: invasive margin; iTIL: intratumoural tumour-infiltrating lymphocytes; OR: odds ratio for 5 years overall survival; p: statistical significance by multivariable binary logistic regression; sTIL: stromal tumour-infiltrating lymphocytes.
DISCUSSION AND CONCLUSION
Compartmental morphological analysis of TIL reveals frequent intermediate to high density of TIL content on IM and their overall statistically significant prognostic impact. This draws attention to this neglected tumoural compartment and directs the question towards the different biology, cell composition, and role of each tumour morphological compartment, a phenomenon that should definitely be further explored.








