BACKGROUND
Breast cancer (BC) is the most common cause of cancer-related deaths in females under 45 years. It has been reported as a more aggressive disease, requires more aggressive treatment, has a poorer survival rate, and leads to more serious psychosocial consequences. Evidence about the epidemiology, biologic behaviours, and treatment strategies are needed to help clinicians understand this disease. The young female population is under-represented in clinical studies and therefore, real-world data could be useful in broadening knowledge and aiding management of patients.
METHODS
The authors conducted a retrospective study, selecting patients aged ≤45 years with BC diagnosis in the Breast Cancer Unit of Puerta de Hierro Hospital, Majadahonda, Spain between 2014 and 2019. Epidemiological, clinical, and pathological information was collected. The aim was to understand the characteristics of the breast cancer in young females (BCYF) patient population and to assess the quality of care of the diagnostics and treatments.
RESULTS
A total of 348 patients with diagnosis of BC were selected; median age was 41 years (range: 38–44 years) with the majority (61%) aged 41–44 years.
Clinical and epidemiological characteristics of the patient cohort are described below: 79.9% of the patients had a previous pregnancy and almost half (49.0%) breastfed. Of the patients studied, 52% had never smoked, with this percentage being higher in the <35 years subgroup (68.8%). Regarding oral contraceptive intake, 44.3% of patients had used them at some point in their life, which increased to 54.6% in the <35 years subgroup. Median BMI was 22.8. In relation to family history, 32.0% had a history of breast cancer and 4.6% had a history of ovarian cancer. A BRCA 1/2 mutation was carried by 7.4% of the patients; this percentage reached 21.1% in the <35 years subgroup.
Analysis of the histological characteristics revealed results as follows: the most common histological type was ductal (84.5%) followed by lobular (8.3%), with no significant differences between age subgroups. The hormone receptor positive (HR+)/human epidermal growth factor receptor 2 negative (HER2-) subtype was the most prevalent (69.5%), followed by HR+/HER2+ (14.3%); 11.2% were triple-negative and only 5% were HER2+/HR-. Most of the patients presented at Stage I or II (38.1% and 38.4%, respectively); 18.6% presented at Stage III and 4.9% were metastatic at diagnosis (data consistent with literature). In relation to axillary staging, 43.8% were positive at diagnosis and this was similar between the three subgroups.
CONCLUSIONS
In our BCYF cohort, no association was found between age groups and clinical or pathological characteristics, which differs from other previously published studies reporting a poorer prognosis in young females.
The cohort distribution, per stages and subtypes, was similar to the global population described in the medical literature. This suggests the need for a detailed BCYF analysis to find evidence for the specific management of this population, and to prevent age-related disparities in BC care.
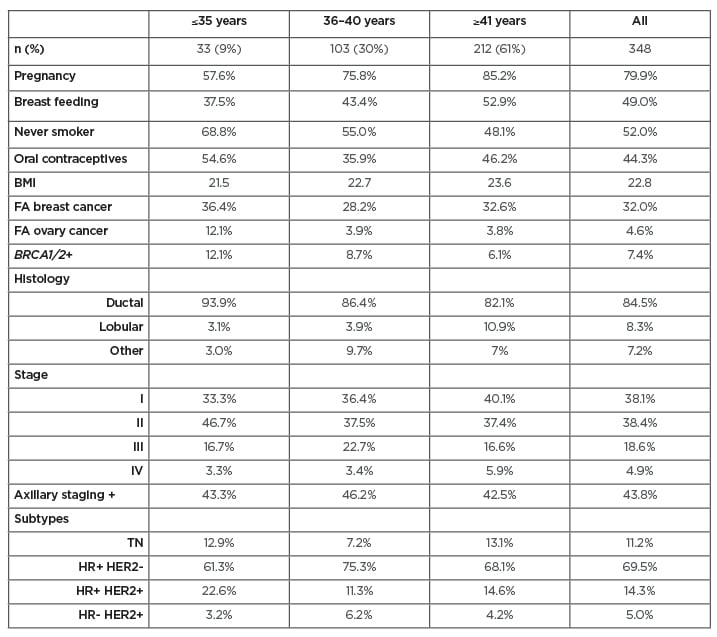
Table 1: Clinical and pathological characteristics of breast cancer in the young females’ cohort.
FA: fibroadenoma; HER2: human epidermal growth factor receptor 2; HR: hormone receptor; TN: triple negative.








