Abstract
Background: The authors aimed to study the levels of anxiety, depression, and stress in survivors of COVID-19, and to correlate their level with severity of COVID-19 infection.
Methodology: This study was conducted on a total of 200 survivors of COVID-19 as an observational cross-sectional study. The cohort reported to the Hamidia Hospital, Bhopal, India, during the study period of 21 months. The Depression Anxiety Stress Scale-21 (DASS21) was used for assessment of mental health.
Results: Overall, depression, anxiety, and stress were observed in 38.5% of cases, 38.5% of cases, and 11.0% of cases, respectively. The authors reported a significant association of worst saturation recorded with depression and severity of depression (p<0.05); significant association of depression and severity, and anxiety and its severity; and severity of stress with moderate-to-severe high-resolution CT findings (p<0.05). The authors also documented a medium positive and significant correlation of the severity of COVID-19 infection with stress and DASS21 overall score (analysis of variance: r=>0.40; p<0.05). However, a weak positive but significant correlation of severity with depression and anxiety was noted (r=0.20–0.40; p<0.05). The authors reported a weak positive correlation of worst saturation with depression and anxiety, as well as overall DASS21 score (r=0.20–0.40; p<0.05).
Conclusion: COVID-19 has long-term effects, especially in the form of psychological morbidity. Patients have recovered from the physical illness, but psychological distress and mental problems are still persistent among the survivors as the prevalence of depression, anxiety, and stress is reported to be high among them.
Key Points
1. The COVID-19 pandemic had a devastating impact on the lives of individuals worldwide. The impact was not only seen on health, but also day-to-day activities. It significantly changed the normal course of life of an individual.
2. The authors present a cross-sectional observational study for the assessment of the mental health of survivors of COVID-19.
3. All survivors of COVID-19 must be screened for mental problems periodically, as these illnesses may significantly negatively impact their quality of life.
INTRODUCTION
COVID-19 infection was first reported in December 2019 in Wuhan, China, as a pneumonia outbreak presenting with fever, cough, body ache, dyspnoea, etc.1 The COVID-19 pandemic resulted from a novel coronavirus infection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).2 As of 21st July 2022, a total of 567 million cases and 6.3 million deaths were reported across the world.3 In India, 43.8 million people were affected, and 528,000 deaths were reported in the same period.4
Psychological health was affected during the pandemic, as there is distress and uncertainty regarding one’s own health, due to the absence of proper management and availability of beds during the ongoing pandemic. Also, the situation was further worsened by the quarantine of patients away from their families, prolonged hospital stays, panic due to social media posts about the pandemic, and false or unverified information. These may be the factors associated with high levels of psychological and mental stress among individuals.5,6 The research to date has mainly focused on assessing mental health among medical staff, doctors, and the general population amidst the COVID-19 pandemic.7,8 However, the mental health status of patients with COVID-19 who suffered from the illness and trauma of isolation in quarantine wards and COVID-19 care centres has not been explored much. Recently, a few researchers highlighted the negative impact of COVID-19 on mental health and quality of life among survivors, which may be an indicator of prognosis in such patients.9,10
Previous studies have reported that mental illnesses such as anxiety, depression, and post-traumatic stress disorders (PTSD) are common among survivors of COVID-19.11-13 The mental health status of survivors of COVID-19 may remain affected even after discharge, and the pandemic may have long-term chronic effects on the mental health status of patients.14 Addressing the impact of COVID-19 on the mental health status of survivors of COVID-19 is essential for improving their overall health status. With the above background, the present study was conducted at a tertiary care centre in India to study the level of anxiety, depression, and stress in survivors of COVID-19, and to correlate the level of depression, anxiety, and stress in individuals who had recovered from COVID-19 with the severity of infection.
MATERIALS AND METHODS
The Department of Medicine and Psychiatry at Gandhi Medical College and associated Hamidia Hospital, both in Bhopal, India, conducted a cross-sectional observational study from January 2021–September 2022. The study population includes Indian patients who visited the psychiatry and medicine outpatient department; who had tested positive for COVID-19 infection in the past 6 months using a rapid antigen test kit and/or reverse transcription-PCR test; who were admitted for 3 or more days for their illness; and who had subsequently recovered. Patients aged 18 years and above who consented to participate in the study were included. However, the study had certain exclusion criteria. Patients with a past history of psychiatric disorders or any other psychiatric disorder were excluded from the study.
Data Collection Method
After obtaining ethical clearance from Gandhi Medical College and Hamidia Hospital’s Ethical Committee, all the patients fulfilling the inclusion criteria and giving written consent for participation were enrolled in the study. Detailed history regarding sociodemographic variables; their current complaints; and comorbid conditions, such as diabetes, hypertension, or any respiratory illness, was obtained and documented. Detailed history regarding previous COVID-19 infection and investigation workup was obtained. Their past records and data regarding the findings of high-resolution CT (HRCT) chest, and worst O2 saturation (severe illness: saturation of peripheral O2: <94% on room air) were accessed. A CT severity score was assigned out of 25, based on the percentage area involved in each of the five lobes. The total CT score is measured by the sum of the individual lobar scores, and can range from 0 (no involvement) to 25 (maximum involvement) when all five lobes show more than 75% involvement. CT severity scores of 1–5, 6–14, and 15–25 were categorised as mild, moderate, and severe involvement, respectively.
Psychiatric conditions in such patients were assessed using the Depression Anxiety Stress Scale-21 (DASS21),14 with 21 items (Figure 1).15 The scale is based upon the dimensional concept of psychological disorder rather than categorical conception.15
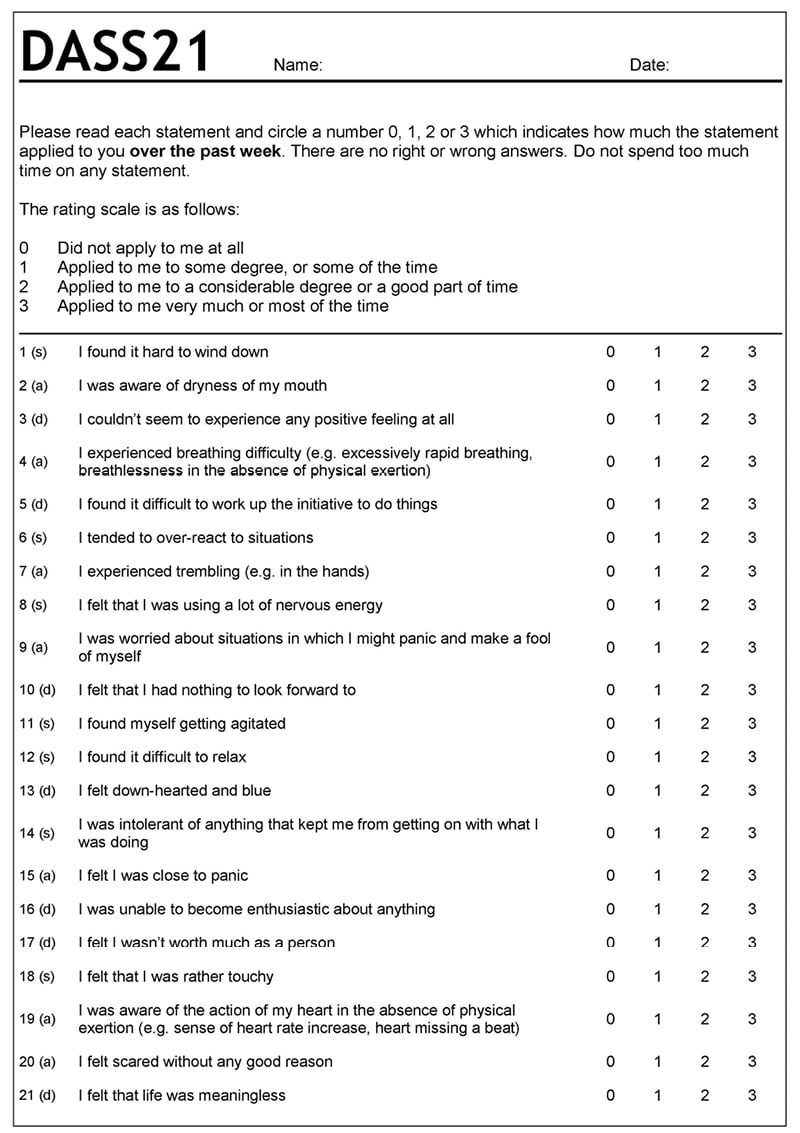
Figure 1: Psychiatric conditions were assessed using the Depression Anxiety Stress Scale-21.
Scores on the DASS21 are multiplied by 2 to calculate the final score.
DASS21: Depression Anxiety Stress Scale-21
Statistical Analysis
Data was compiled using Microsoft Excel (Microsoft, Redmond, Washington, USA), and analysed with the help of IBM® (Armonk, New York, USA) SPSS software version 20. Categorical data was expressed as frequency and proportion, whereas continuous data was expressed as mean and standard deviation. The association of mental disorders with the severity of infection was done using the χ2 test, and correlation was done using the Pearson correlation coefficient. A p value of less than 0.05 was considered statistically significant.
RESULTS
The study was conducted on a total of 200 survivors of COVID-19, with a mean age of 39.370±12.938 years. Male predominance was observed with a male:female ratio of 1.3:1.0. Approximately 74% of survivors of COVID-19 belonged to middle socioeconomic status. The most common comorbid condition observed among the group was diabetes (19.5%), followed by hypertension (17.0%).
The mean saturation (worst) recorded among survivors of COVID-19 was 91.220±5.385%. Approximately 2.5% of cases had saturation below 80, whereas 40.0% had saturation in the 80.0–90.0% range. HRCT was suggestive of mild severity in 53.0% of cases, whereas CT severity score was moderate and severe in 16.5% and 2.0% of cases, respectively.
Mean depression, anxiety, and stress scores were 11.220±6.490, 6.060±3.513, and 7.950±3.007, respectively. Overall, depression was observed in 38.5% of cases, and the majority of cases had mild (21.0%) and moderate (17.0%) depression. However, anxiety was noted in 38.5% of cases, and the majority of patients had mild anxiety (21.0%), followed by moderate anxiety (17.0%). Stress was present in 11% of cases, and the majority had mild stress.
The authors reported a significant association of worst saturation recorded with depression and severity of depression (p<0.05; Table 1). They also documented a significant association between depression and its severity and anxiety and its severity; and severity of stress with moderate-to-severe HRCT findings (p<0.05; Table 2)
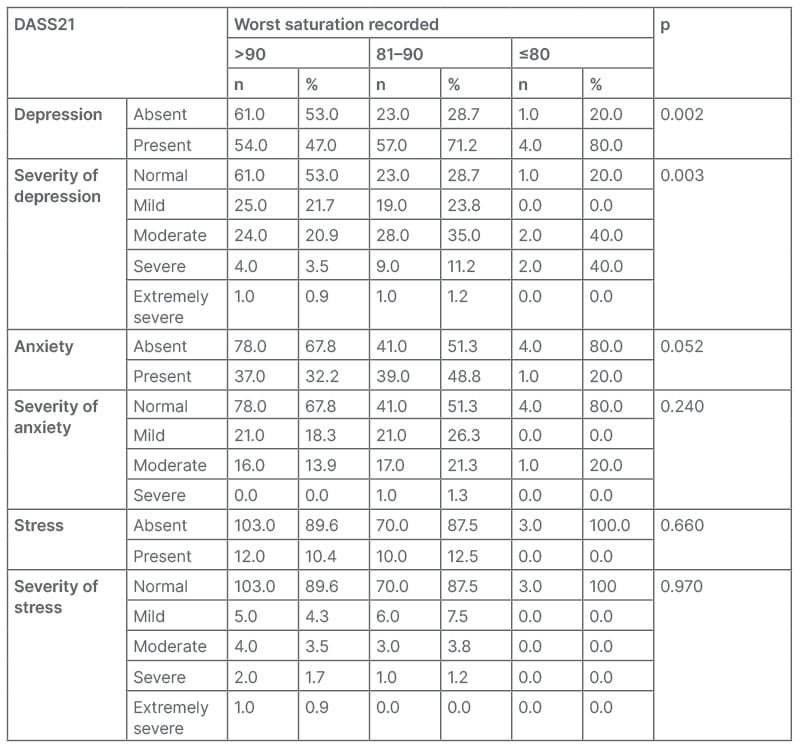
Table 1: Association of Depression Anxiety Stress Scale-21 with worst saturation recorded.
DASS21: Depression Anxiety Stress Scale-21.
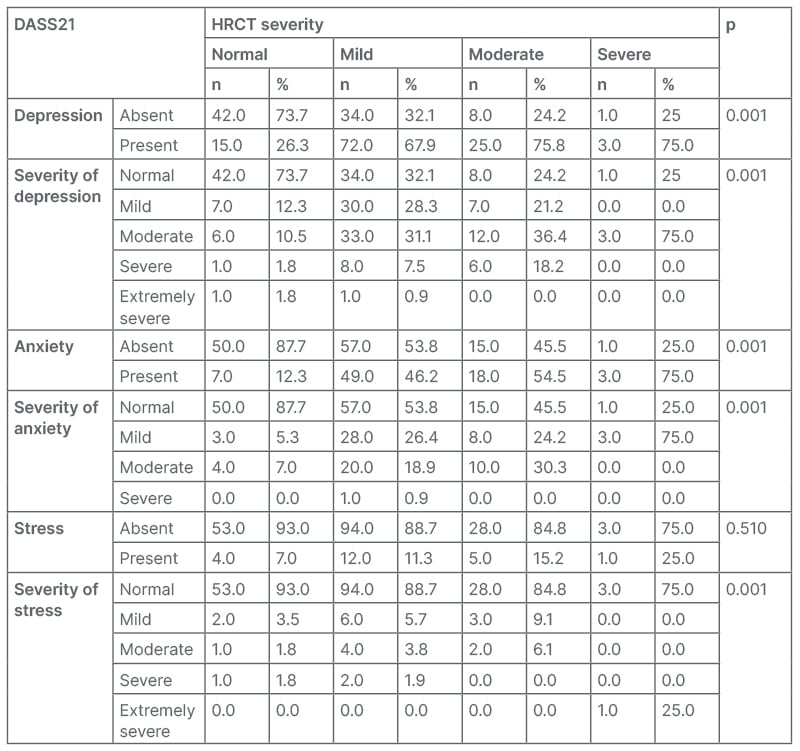
Table 2: Association of Depression Anxiety Stress Scale-21 with high-resolution CT severity.
DASS21: Depression Anxiety Stress Scale-21; HRCT: high-resolution CT.
The authors documented a medium positive and significant correlation between the severity of COVID-19 infection with stress and DASS21 overall score (analysis of variance: r=>0.40; p<0.05). However, a weak positive but significant correlation of severity with depression and anxiety was noted (r=0.20–0.40; p<0.05). They reported a weak positive correlation of worst saturation with depression and anxiety, as well as overall DASS21 score (r=0.20–0.40; p<0.05; Table 3 and Table 4).
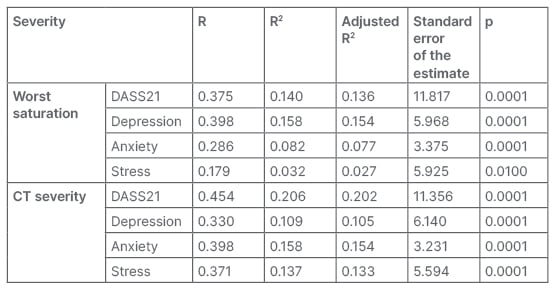
Table 3: Correlation of severity of COVID-19 with Depression Anxiety Stress Scale-21.
DASS21: Depression Anxiety Stress Scale-21; R: Pearson’s correlation coefficient; R2: used in analysis
of variance.
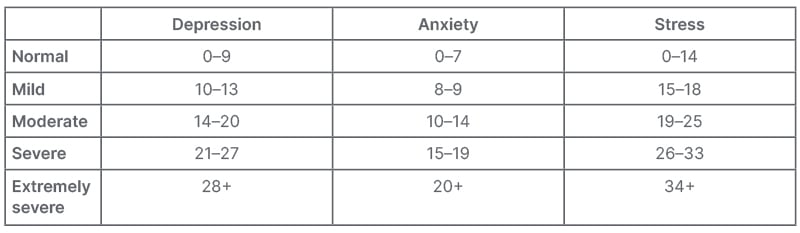
Table 4: Severity of depression, anxiety, and stress.
DISCUSSION
The COVID-19 pandemic was a dreadful pandemic, which had a devastating impact on almost all aspects of health. Though the waves of the pandemic have subsided, the literature suggests that the pandemic may have a long-term impact on the mental health of survivors of COVID-19, who might have faced immense trauma due to illness itself, isolation from family and friends, fear of death, etc.10,11 Post-traumatic stress disorders (PTSD), depression, anxiety, etc. are documented among survivors of an outbreak.9-11 The authors aimed to assess the level of depression, anxiety, and stress in survivors of COVID-19, and to correlate these problems with the severity of infection. The authors used the DASS21 scale for the assessment of mental disorders among the survivors, which is a valid and reliable scale for the assessment of depression, anxiety, and stress, with Cronbach’s alpha values of 0.66, 0.29, and 0.52, respectively.16
COVID-19 infection was associated with various short-term and long-term morbidities among survivors. Psychological problems, including depression, anxiety, and stress have been reported to be common in patients who have recovered from COVID-19 infection.16 The action of coronavirus infection on angiotensin-converting enzyme 2 (ACE2) receptors in the central nervous system (CNS) may lead to neurological symptoms. However, the role of cytokine storm associated with the infection has also been postulated.17
In the CNS, ACE2 is expressed in a physiologically appropriate manner. Whether ACE2 expression is increased in pathological situations like SARS-CoV-2 infection is unknown. The presence of ACE2 in the CNS makes it possible for SARS-CoV-2 to invade neuronal cell membranes and cause neurological symptoms, as well as brain damage. A previous coronavirus study suggested that the coronavirus attaches to target cells’ surfaces when the S1 unit of the spike protein on its surface interacts with the ACE2 receptor on neurons.17 The spike protein is then activated by transmembrane protease, serine 2, which allows the virus to enter the neuron. Moreover, SARS-CoV-2 infection can attack endothelial cells in cerebral blood vessels via the ACE2 receptor and disrupt the blood–brain barrier (BBB), leading to increased BBB permeability, cerebral oedema, and intracranial hypertension. Endothelial cells of blood vessels also express ACE2 at high levels. A compromised BBB may also encourage invasion into neurons and brain tissues. One of the major causes of a higher proportion of mental illness is social isolation as a result of infection, leading to loneliness and grief after bereavement, and financial worries. Vice versa, patients with pre-existing mental illness were more likely to get infected, and hospitalisation and death were reported to be higher among them.18
The authors reported depression in 57.5% of survivors of COVID-19, with severe and extremely severe depression in 7.5% and 1.0% of cases, respectively. Anxiety was documented in 38.5% of cases with mild-to-moderate anxiety in the majority of cases. Stress was reported in 11.0% of cases: mild in 5.5%, moderate in 3.5%, severe in 1.5%, and extremely severe in 0.5%.
As the study participants were from a younger age group and did not have a significant past history of any respiratory illness, specifically chronic obstructive pulmonary disease, that could also change the overall burden of psychiatric illness in this study, as anxiety, depression, and stress have been associated with lung diseases, specifically chronic obstructive pulmonary diseases.
In this study, diabetes and hypertension were the common comorbidities observed in 19.5%, and 17.0% of survivors of COVID-19, respectively. Siddiqui et al.19 reported diabetes, hypertension, chronic lung disease, and coronary artery disease in 61.5%, 47.1%, 3.8%, and 24.0% of survivors of COVID-19, respectively.
These study findings were supported by the findings of Shah et al.,20 who reported anxiety and depression in 68.7% of survivors of COVID-19. Khademi et al.16 reported anxiety, depression, and PTSD in 5.8%, 5.0%, and 3.8% of survivors. Uvais et al.21 reported depression, anxiety, and PTSD in 26.2%, 12.1%, and 3.7% of cases, respectively. Huang et al.22 reported the prevalence of anxiety, depression, and PTSD after 12 months of infection as 6.26%, 11.94%, and 6.07%, respectively. Chen et al.23 documented the prevalence of depression at 21.0%, anxiety at 16.4%, and PTSD at 13.2% among patients with COVID-19 who were hospitalised.
The correlation of health disorders was assessed with respect to the severity of infection. The severity of the infection was determined using the worst saturation and CT severity score. In this study, the worst saturation below 80% was significantly associated with depression, as well as increased severity of depression; whereas HRCT severity showed a significant association with depression as well as anxiety, with increasing severity of depression, anxiety, and stress (p<0.05). The authors also documented a moderate positive statistically significant correlation between the severity of COVID-19 infection with stress and DASS21 overall score (r=>0.40; p<0.05). However, a weak, significant correlation of severity with depression and anxiety was noted (r=0.20–0.40; p<0.05). These study findings were supported by the findings of Parker et al.,24 in which the authors documented a higher rate of PTSD in cases with severe physical illness (not particularly COVID-19). The present study’s findings are concordant with the findings of Liu et al.,7 in which mental and neurological disorders among survivors were significantly associated with the severity of illness. Similarly, Magnúsdóttir et al.25 in their study documented a significantly higher risk of depression, as well as anxiety, in patients with COVID-19 who were bedridden for more than 7 days, as compared with patients who were not bedridden (p<0.05). Pappa et al.26 found that the majority of cases suffered from severe COVID infection (48.25%), followed by 34.97% and 13.99% with moderate and critical illness, respectively.
LIMITATION
The present study was conducted as an observational cross-sectional study; however, a prospective study with follow-up of patients after discharge might have revealed the long-term outcomes.
Since this study was cross-sectional, there is no comparison/control for people who lived through the COVID-19 pandemic with the same stresses, and there is no baseline data on mental health disorders, which may bias the result.
This is a limited and selective sample of patients, which does not appear to control for variables such as false or unverified information; this would also be impacting people who have not had the COVID-19 virus.
CONCLUSIONS
COVID-19 has long-term effects, especially in the form of psychological morbidity. Patients have recovered from the physical illness, but psychological distress and mental problems are still persistent among the survivors as the prevalence of depression, anxiety, and stress is reported to be high among them. Mild illness is less likely to have an impact on the mental health of affected individuals, but severe illnesses have been linked with a higher risk of long-term mental health morbidities. All survivors of COVID-19 must be screened for mental problems periodically, as these illnesses may significantly negatively impact the quality of life of the affected individual, and their family members.