Abstract
Central fever, or hyperthermia of central origin, is a not so rare cause of hyperthermia in neurological rehabilitation units, characterised by persistent fever without any recognisable cause, and poor response to conventional antipyretics. This article reports a case of central fever in a patient with tuberculous meningitis, treated with dopamine agonist bromocriptine in conventional doses, which resulted in fever remission. The current literature is also reviewed.
Key Points
1. Central hyperthermia in neurological diseases is a diagnosis of exclusion, postulated to be due to dysfunction of central temperature regulatory mechanisms. The treatment of this condition is empirical, and largely based on anecdotal evidence. Even the commonly used drugs like bromocriptine, baclofen, propranolol, etc., have different dosing regimens in literature. This article attempts to revisit the literature, and suggest a low-dose treatment option.2. The authors present a case of central fever in a patient with tuberculous meningitis and neurological disability, treated with dopamine agonist bromocriptine in smaller doses, which resulted in fever remission. The authors also reviewed the different treatment options for central fever available in literature.
3. Central hyperthermia shall be considered as a differential diagnosis in a patient with central neurological diseases, presenting with fever refractory to other measures. A few treatment options are available with limited evidence. Bromocriptine is an effective agent as per the authors’ experience in the case described. Other options are also available in the literature, which clinicians can choose based on their experience and availability.
INTRODUCTION
Fever is a common medical issue encountered in neurorehabilitation units. The most common cause of fever is infection; the common sources could be genitourinary tract, respiratory tract, gastrointestinal system, skin and soft tissue, and so on. The presence of fever in such patients warrants a rigorous search for the possible source of infection. Immune system impairment, which is observed after any central nervous system insult, also contributes to higher chances of infection. In addition to infections, hyperthermia can be related to the underlying brain insult. The common causes of such central hyperthermia are subarachnoid, intraventricular, and intracerebral haemorrhages; central nervous system tumours; traumatic brain injury; ischaemic stroke; tuberculous meningitis; traumatic spine injuries; and so on. Central hyperthermia is characterised by rapid persistent elevation of temperatures, with marked fluctuations and poor response to the conventional antipyretics. It may be the result of damage or dysfunction of central temperature control centres, which can dysregulate the thermoregulation.1 Fever due to any cause will adversely affect the prognosis of patients with neurological injuries,and need to be addressed with appropriate treatment strategies.
In this paper, the authors present a 35-year-old male with persistent central fever after a tuberculous meningitis and obstructive hydrocephalus. The fever was difficult to control with the conventional antipyretics,but responded well with the conventional doses of bromocriptine.
PATIENT INFORMATION
A 35-year-old male with no significant pre-existing illnesses presented with acute headache, dizziness, vomiting, and mild left-sided weakness. CT examination revealed supratentorial hydrocephalus, atlantoaxial hemispinal deformity with basilar invagination, and multiple left cervical chain lymph nodes. MRI confirmed the ventriculomegaly and narrowing of the spinal canal at C1 level, with compressive myelopathy at the cervical-medullary junction (Figure 1), along with basilar invagination and atlantoaxial subluxation. External ventricular drainage of cerebrospinal fluid (CSF) was done, which revealed lymphocytic predominant leucocytosis, and tuberculous bacilli DNA was isolated.
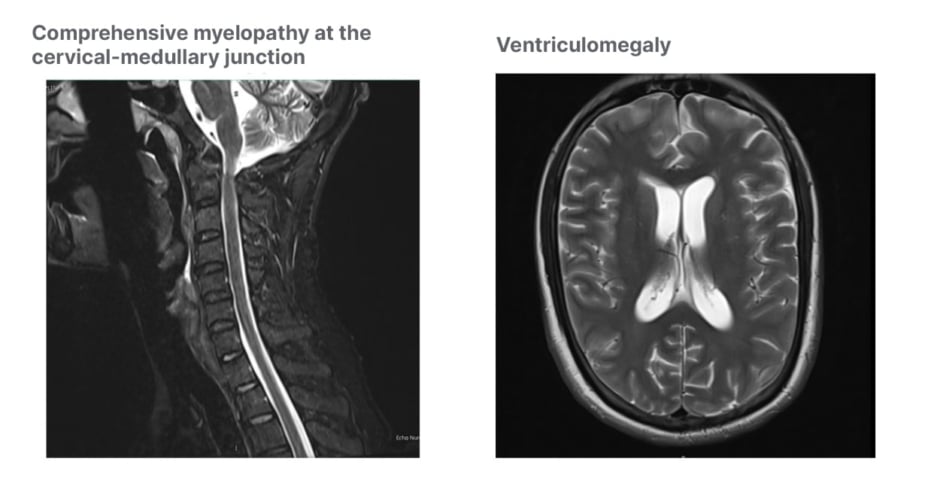
Figure 1: Compressive myelopathy with obstructive hydrocephalus.
The patient was started on the conventional four-drug regimen for extra-pulmonary tuberculosis (rifampicin, isoniazid, pyrazinamide, and ethambutol). He started to vomit,and was noted to have a rising trend of transaminases while on first-line agents. Hence, the first-line agents were stopped, and he was started on second-line agents (amikacin, moxifloxacin, cycloserine, and linezolid). Vomiting subsided, and transaminase level improved.
CLINICAL FINDINGS AND DIAGNOSTIC ASSESSMENT
The patient developed another episode of fever with desaturation. Blood pressure, pulse rate, and respiratory rate were normal. General examination was unremarkable, except mild pallor. Cardiorespiratory examination, abdominal examination, and genitourinary examination did not reveal any abnormalities. Neurological examination showed generalised weakness, wasting with normal reflexes, and normal sensorium. Higher mental functions and cranial nerves functioned normally. Blood culture showed Klebsiella pneumonia, but no source could be identified despite extensive search. He was treated with ertapenem as per sensitivity for 14 days, but fever persisted. Blood cultures after that failed to demonstrate any further growth. Chest X-ray, abdominal ultrasound, and echocardiogram were normal. The patient was otherwise vitally stable, and labs did not reveal any significant pathology. CT scan of the head was repeated to rule out any occult subdural empyema. It showed an interval increase in the size of the supratentorial ventricular system, with no evidence of any infection, and no change in previous findings. Those findings were reviewed by the neurosurgeon to rule out any neurosurgical interventions.
THERAPEUTIC INTERVENTION AND OUTCOME
Since there was no clear focus of infection despite extensive work-up, the team decided to treat him as hyperthermia of central origin,and started him on bromocriptine 2.5 mg daily in divided doses. Fever started trending down from the next day, and no further fever spikes happened (Figure 2). Bromocriptine was continued at the same dose for a period of 3 weeks, and then tapered off and discontinued. There was no fever recurrence, and other vitals and laboratory parameters were within normal limits. Also, no significant side effects in relation to bromocriptine use were noticed.
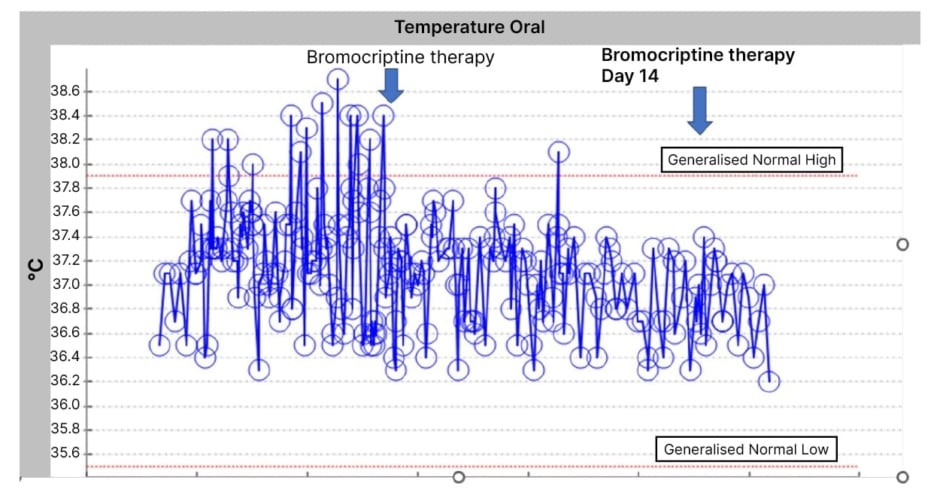
Figure 2: Temperature trend after bromocriptine therapy.
DISCUSSION
Fever or hyperthermia, defined as oral temperature greater than 37.5 °C, is a common situation in patients who have suffered neurological injuries, and are undergoing rehabilitation.2 Fever is a symptom of which differential diagnoses are extensive, the most common being infective aetiology. Common differential diagnosis of fever happening in a rehabilitation unit are enumerated in Table 1, but this is not an exhaustive list. Persistent fever can adversely affect the neurological outcome, extend the length of stay, increase the cost of care, and sometimes can lead to non-judicious use of broad-spectrum antibiotics, leading to microbial resistance.
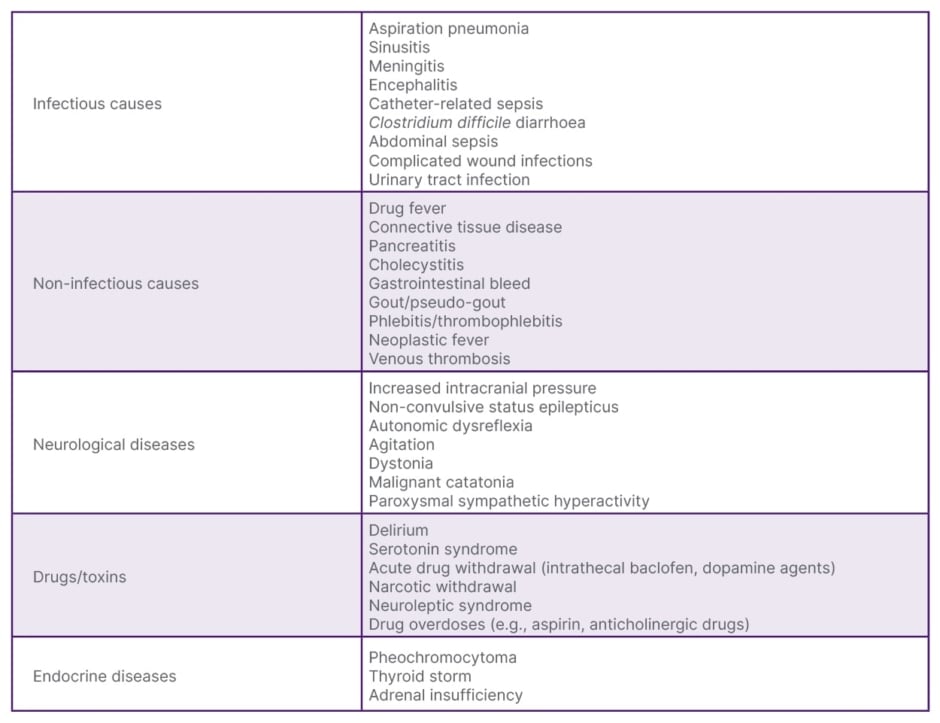
Table 1: Differential diagnosis of fever.
Hence, making an early diagnosis and instituting appropriate management is imperative.
Central fever, also known as neurogenic fever or hyperthermia of central origin, is a not so rare cause of fever encountered in rehabilitation units.3 It can occur alone, or as part of the clinical syndrome of paroxysmal sympathetic hyperactivity. It is characterised by rapid-onset persistent fever, with marked fluctuations and poor response to conventional antipyretics.4 It was first described in 1939 by Theodore C. Erickson.
The origin of central fever is hypothesised to be due to the involvement of central thermoregulatory pathways mediated by various hypothalamic centres, like the lateral parabrachial nucleus and pre-optic area. The pathways involving the brain stem have also been described, which play a role in the pathogenesis of central fever.1 The subject has all probability of either of these areas having been affected by his obstructive hydrocephalus, causing the compression of the brain stem, and a chronic central nervous system infection with associated inflammatory damage.
Central fever is a diagnosis of exclusion. Most common neurologic injuries predisposing to central fever are brain haemorrhages, traumatic brain injury, ischaemic stroke, tuberculous meningitis, and so on. A high index of suspicion is warranted when any patient with above neurological conditions presents with persistent high-grade fever, negative cultures, no definite identifiable source, and failure to respond to conventional antipyretics. Sometimes the coexistence of another infection or physiologic stress of neurologic insult can lead to an elevation of inflammatory markers and leucocytosis, which can cloud the diagnosis. However, the inflammatory response will be of a lower grade compared to infections, and the response to empirical antibiotic therapy will not be observed in central fever.
Controlling fever is important, due to the negative effects of hyperthermia in the injured brain. Since the response to conventional antipyretics has been poor, other methods have been explored in the management of central fever. Several physical methods have been tried with limited efficacy, and sometimes with patient discomfort. They include rotary fans, sponging, surface cooling devices, hypothermia blankets, intravenous infusion of cold saline, inhaled cooling systems, and local brain cooling systems. Various medications have also been tried anecdotally, including morphine, chlorpromazine, baclofen, bromocriptine, growth hormone, and IL-1 antagonists.5
Bromocriptine is a dopamine D2 agonist that acts on the hypothalamus and corpus striatum, and has shown some effect in symptomatic management of paroxysmal sympathetic hyperactivity.6 There are no systematic studies regarding the use of bromocriptine in central hyperthermia; however, a few case reports have demonstrated some benefit using different doses of bromocriptine.7 In a case report, a patient with traumatic brain injury and high-grade fever, diagnosed as central hyperthermia, was treated with 0.025 mg/kg bromocriptine, which was later increased to 0.05 mg/kg. A comparison of mean daily temperatures before and after bromocriptine revealed significant lowering of body temperature, and the patient was weaned off over the next 5 weeks without any relapse of fever.8 Other similar case reports have been reported in the literature.9-11
CONCLUSION
This case report describes a case of central hyperthermia managed with a minimal dose of bromocriptine. Central fever should be considered as a possible differential in any patients who are neurologically injured, in which no other source for hyperthermia is identified. Bromocriptine could be an effective therapeutic option, but more structured studies are needed to evaluate its efficacy and safety in the management of central fever.
STRENGTH AND LIMITATIONS
As mentioned elsewhere, central hyperthermia is a challenging clinical entity, and not many pharmacological agents have been identified conclusively of any benefit. The researchers used bromocritine based on anecdotal reports, but with lesser doses, and became successful in managing the patient. Identifying the role of bromocriptine, even in small doses, could open the door for identifying other agents with a similar mechanism of action in the management of central hyperthermia. Having said that, this being a single case, it has limited value to suggest it as a therapeutic agent to be included in management algorithms of central fever.
PATIENT PERSPECTIVE
Once the fever started settling down, the patient started participating in the therapies well, which translated to better functional gains at discharge. His psychological state also improved, and he expressed his pleasure at the outcome of treatment. He finished his rehabilitation successfully, and was discharged from the inpatient rehabilitation service after he attained all the functional goals.







