Abstract
Background: It is essential to address psychological health, particularly post-traumatic stress disorder (PTSD), among patients who have recovered from COVID-19. The negative impacts on the psychological health of an individual have negative impacts on health-related quality of life. The authors aimed to assess PTSD in patients recovered from COVID-19, and COVID-19-related comorbidities.
Methodology: The present study was conducted as an observational cross-sectional study on patients diagnosed with COVID-19 who were discharged from Gandhi Medical College and Hamidia Hospital, both in Bhopal, India, and returning to follow-up at the medicine/psychiatry outpatient department within 6 months after discharge, during the study period of 20 months. Detailed history regarding sociodemographic variables, previous medical history, comorbidities associated with COVID-19 (e.g., mucormycosis, etc.) were noted. PTSD was assessed using the PTSD Symptom Scale (PSS).
Results: A total of 120 cases, who recovered from COVID-19 infection and sought care at the authors’ centre, were included in this study, with mean age of 37.520±12.756 years. Mean PTSD score was 3.350±1.528, and PTSD was noted in 85% cases. Of these, 83.3% cases had mild, and 1.7% cases had moderate PTSD. The authors observed no significant association of sociodemographic variables with PTSD on univariate as well as multivariate analysis (p>0.05).
Conclusions: Though the wave of COVID-19 pandemic has subsided, the long-term morbidities, particularly due to the impact on psychological health, are still persistent. PTSD is a common consequence following recovery from COVID-19 infection. Thus, mental health services must be provided to patients recovered from COVID-19 infection, mainly targeted at prevention of PTSD.
Key Points
1. Articles on post-traumatic stress disorder (PTSD) in patients with past COVID-19 infection are crucial, as they shed light on the psychological aftermath of the pandemic. Understanding and addressing this issue is vital for healthcare professionals to provide appropriate support, to minimise long-term mental health consequences, and to develop effective intervention strategies.
2. This manuscript describes the potential psychological effects, such as PTSD, in patients who have recovered from COVID-19.
3. Clinicians addressing PTSD in patients post-COVID infection should recognise the potential for psychological distress. Early identification, empathetic communication, and tailored interventions can mitigate long-term effects, promoting holistic recovery and improved mental wellbeing.
INTRODUCTION
An outbreak due to a novel strain of severe acute respiratory syndrome coronavirus 2 was reported in China in December 2019, which was observed in all parts of the world rapidly. The World Health Organization (WHO) termed the condition as novel COVID-19, and on 11th March 2020, the WHO declared COVID-19 a pandemic.1 Though the infection had a significant impact on physical health, particularly respiratory illness, in the form of mild-to-severe symptoms, almost all the dimensions of health were affected.2 Patients were kept in isolation away from their family and relatives in intensive care units, high-dependency units, and COVID care centres, depending upon the severity of infection, to prevent the spread of infection. As the mortality rate of the infection was high, especially in the presence of certain risk factors, knowledge regarding such risk factors had significant impact on the person’s perception of the likelihood of death from COVID-19. The impact on mental health was reported not only in COVID-19 patients with risk factors, but also in patients without risk factors.3,4 Also, the outbreak created a state of panic among the general population, and fuelled psychological problems in the form of fear, stress, anxiety, depression, insomnia, irritability, confusion, and stigma associated with quarantine.4-7 Thus, COVID-19 may have been a traumatising experience, which may be associated with psychological and psychiatric symptoms in patients post-COVID-19 infection.3
According to previous literature, fear, stress, anxiety, panic, etc., are natural reactions to any sudden outbreak or global health crisis.8-10 However, recent studies suggest that epidemics and pandemics may have been traumatic experiences for certain individuals, and may result in post-traumatic stress disorder (PTSD), or long-term sequlae in the form of chronic psychological symptoms.11,12 PTSD is a stress-related psychological condition that occurs immediately following traumatic experience, such as severe accident, near-death experience, and sexual or physical violence.13 This occurs when the memories, emotions, or thoughts experienced during the trauma or event re-occur, leading to restrictions and inconvenience in the individual’s day-to-day life.13 Overall, the prevalence of PTSD among individuals who have recovered from COVID-19 infection has been documented to range from 7.0–41.3%.12,14 In addition, the prevalence of PTSD is documented to be higher among residents of highly affected areas compared to individuals living in surrounding areas.11
The impact of COVID-19 infection on the psychological health of an individual in the general population, and health workers, has been explored previously.3,4 It is essential to address the psychological health, particularly PTSD, among recovered patients, as the negative impact on psychological health of an individual has negative impacts on health-related quality of life.14,15 The data regarding the prevalence of PTSD is scarce in recovered cases. The present study was therefore conducted at tertiary care centre to assess PTSD in patients recovered from COVID-19, and COVID-19-related comorbidities.
METHODOLOGY
The present study was conducted as an observational, cross-sectional study on patients diagnosed with COVID-19, who were discharged from Gandhi Medical College and Hamidia Hospital, both in Bhopal, India; and who returned to follow-up at the medicine/psychiatry outpatient department within 6 months after discharge, during the study period of 20 months between January 2021–September 2022. People with documented COVID-19-positive status, who were willing to participate in the study were included, whereas those who already had psychiatric disease or a mental health issue, those not giving consent, and those with prolonged medical and surgical comorbidities were excluded from the study.
Initially, ethical clearance was obtained from the Institute’s ethical committee. Following this, all patients fulfilling inclusion criteria were enrolled, and written consent was obtained. Detailed history regarding sociodemographic variables, such as age, sex, residence, marital status, education, occupation, socioeconomic status, etc., was obtained, and entered in proforma. Each patient was assigned a case code and date of enrolment in the study, and a date of positive report was documented. History regarding comorbidities associated with COVID-19 (e.g., mucormycosis), and social factors associated with illness (COVID-19), etc., were also noted.
PTSD was assessed using PTSD Symptom Scale (PSS). This is a 17-item scale that helps in assessing the presence, as well as the severity of, PTSD.16 For each item, the score ranges from 0–3, depending upon the severity. The global PTSD score is calculated by adding the score of all items. Based upon the score, patients can be categorised as16 having mild PTSD (score 1–13), moderate PTSD (score 14–26), or severe PTSD (score 27 and above).
STATISTICAL ANALYSIS
Data was compiled using Excel (Microsoft, Redmond, Washington, USA), whereas analysis of data was done with the help of SPSS Statistics software (IBM, Armonk, New York, USA), version 20. All categorical variables were represented as frequency (percentage), and continuous variables as mean (standard deviation). Predictors of PTSD were evaluated using univariate and multivariate analysis. P value of less than 0.05 was considered statistically significant.
RESULTS
A total of 120 cases recovered from COVID-19 infection and seeking care at the authors’ centre were included in the study, with a mean age of 37.520±12.756 years.
Approximately 39.2% cases belonged to age range of <30 years and male predominance was observed, with a male:female ratio of 1.1:1.0. About 74.2% cases were married, whereas 25% cases were unmarried, and 0.8% cases were widowed. The majority of patients were university graduates (44.2%), followed by 15.0% postgraduates. About 27.5% cases were unemployed, and 72.5% cases were employed. Comorbidities and social factors were absent in 100% of patients.
Mean PTSD score was 3.350±1.528, and PTSD was noted in 85.0% of cases; of these, 83.3% cases had mild and 1.7% cases had moderate PTSD.
In the present study, the authors observed no significant association of sociodemographic variables with PTSD (p>0.05; Table 1). As documented in Table 2, the authors reported no significant association of PTSD with sociodemographic variables (p>0.05). Multivariate analysis revealed no significant association of sociodemographic variables with PTSD (p>0.05; Table 3).
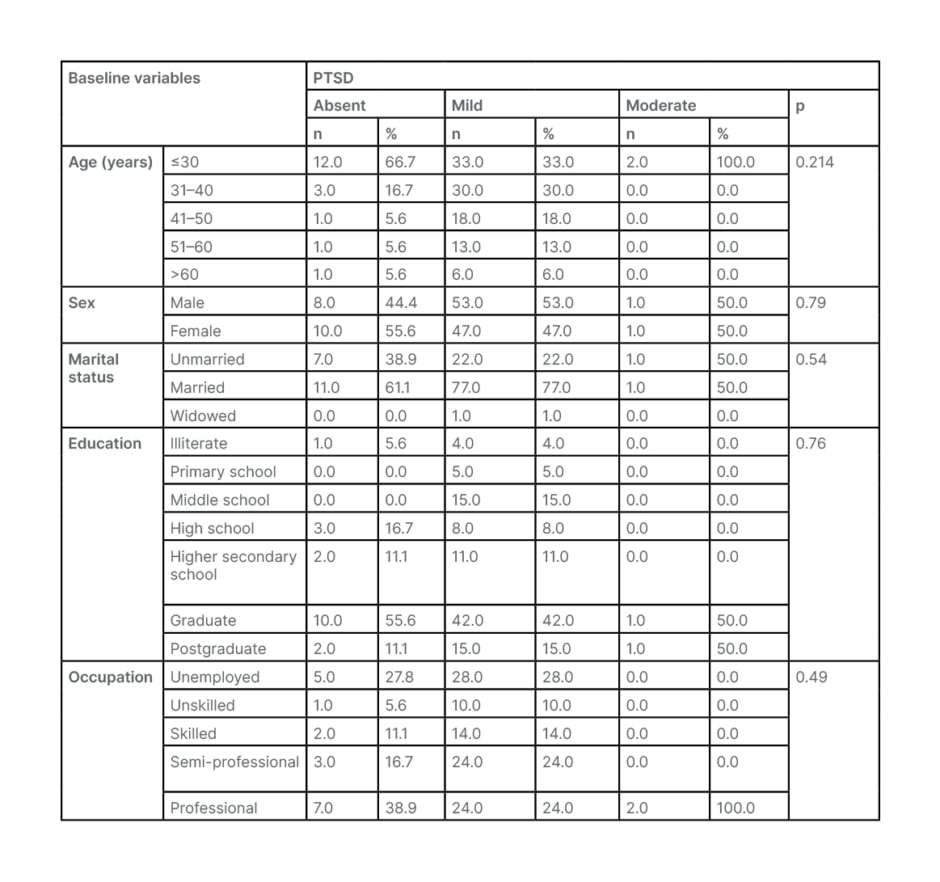
Table 1: Association of post-traumatic stress disorder with sociodemographic variables.
PTSD: post-traumatic stress disorder.
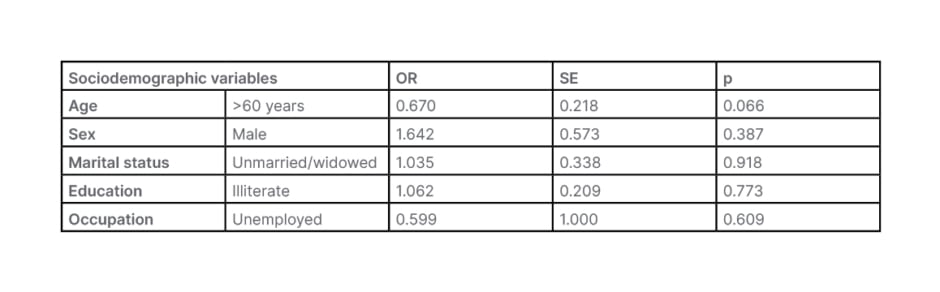
Table 2: Univariate analysis for factors associated with post-traumatic stress disorder.
OR: odds ratio; SE: standard error.
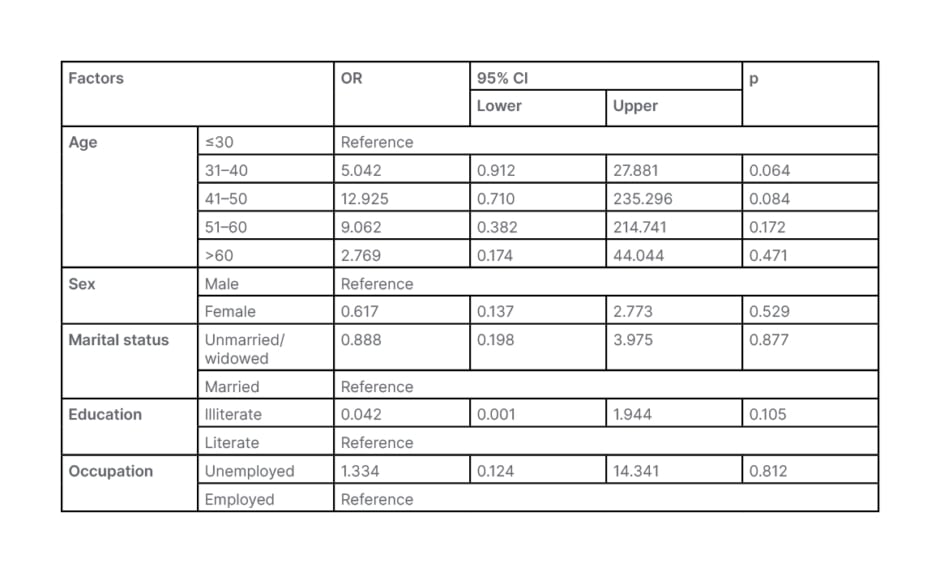
Table 3: Multivariate analysis to determine factors affecting post-traumatic stress disorder.
CI: confidence interval; OR: odds ratio.
DISCUSSIONS
COVID-19, the recent dreadful pandemic, has affected almost all the dimensions of health.2 Though short-term effects of COVID-19 have been studied in various research, in the form of morbidity and mortality, long-term effects are yet to be explored. Patients are finding significant effects on their mental health.3,4 The pandemic has effects on the mental health of an individual, in the form of sleep disturbances, PTSD, and in the form of various psychological problems.11,12 The effect of COVID-19 on psychological health has been addressed among healthcare workers and general population. However, the person experiencing the infection may experience higher psychological harm as compared with the general population. Thus, it is essential to address the psychological health among patients recovered from COVID-19 infection.14,15 The present study was conducted on a total of 120 cases recovered from COVID-19 infection, and seeking care at the authors’ centre. They aimed to assess PTSD among these patients.
COVID-19 infection affected individuals of all age groups, and any gender. All socioeconomic groups of people were affected. However, mortality was documented to be higher in elderly individuals.17 In the authors’ study, mean age of patients recovered from COVID-19 infection was 37.520±12.756 years; the majority belonged to the <30 years of age group. Only 5.8% cases were elderly in the authors’ study. They reported slight male predominance, with 51.7% males and 48.3% females. However, about 44.2% cases were graduates, and the majority were employed in professional work (27.5%).
The authors’ study findings were supported by findings of Fu et al.,18 in which 29.6% cases belonged to the 31–40 years of age group, about 56.3% cases were females, 43.2% cases achieved education up to college level or above, and 40.2% were engaged in full-time employment. However, the mean age of patients in a study of Sun et al.19 was higher as compared with the present study (55.7±13.7 years), with male predominance similar to the authors’ study. Mean age of patients recovered from COVID-19 infection was 57.67±11.42 years, and the majority (60.6%) of cases were females in a study of Huang et al.20 The majority of cases in a study of Pérez-Carbonell et al.21 were females, who were middle aged (median age: 52.0 years).
PTSD is characterised by psychiatric symptoms development, particularly following a traumatic event.22 The cause of PTSD among survivors has been linked with bad experience such as near-death experiences, delirium, and trauma.23 Hypoxic brain injury may be linked with PTSD.24 Further, altered circadian rhythm, intensive care admission, intensive care psychosis, and poor sleep quality may also be factors associated with PTSD, even after discharge.25 PTSD was assessed using PSS. The authors documented PTSD in 85.0% of cases, with mean PTSD score of 3.350±1.528. All the cases had mild PTSD, except two (1.7%) who had moderate PTSD.
Sun et al.19 observed PTSD in 22.6% survivors of COVID-19. Tu et al.26 documented higher proportions of PTSD among survivors of COVID-19 as compared to controls. Janiri et al.27 reported PTSD in 30.2% cases. Huang et al.20 documented much lower prevalence of PTSD (11.5%).
In the present study, the authors observed no significant association of sociodemographic factors, such as age, sex, marital status, occupation, and education with PTSD (p>0.05). Boyraz et al.28 suggested that sociodemographic variables, such as age, sex, fear of job loss, and financial loss may be associated with PTSD. Patients who developed symptoms of PTSD reported a significantly lower health-related QoL compared to patients without PTSD.29 The main factors associated with the development of PTSD-related symptoms were a higher education level, a lower monthly income, and more than two comorbidities.29 Female sex was associated significantly with high risk of PTSD using the Impact of Event Scale – Revised (IES-R) in a study of Pappa et al.30 Janiri et al.27 also documented female sex to be significantly associated with PTSD (p<0.05). Female sex was associated with higher risk of PTSD in a study of Huang et al.20 Social support had a weak association with mental disorder symptoms during the COVID-19 pandemic, while the association with loneliness was moderate. Strategies to address loneliness could be highly effective in reducing the impact of the pandemic on social relationships and mental health.31
The authors’ study had certain limitations; first, the sample size was small, and the majority of cases presented in this study suffered from mild-to-moderate disease. However, the incidence of PTSD might have been higher in cases with severe or critical disease.
CONCLUSIONS
Though the wave of the COVID-19 pandemic is subsided, the long-term morbidities, particularly due to the impact on psychological health, are still persistent. PTSD is a common consequences following recovery from COVID-19 infection. Thus, mental health services must be provided to patients who have recovered from COVID-19 infection, mainly targeted at the prevention of PTSD.







