Resistance to eye opening (REO) is defined as strong closure of already closed eyelids by a patient when they are touched by an examiner during ophthalmological examination. REO has been described in many different disorders, such as psychiatric coma, non-epileptic attacks, stroke, anoxia, and demyelinating illness.1-3 Explanations for this symptom range from wilful to reflexive. As empirical data regarding REO in severe brain-injury patients with chronic disorders of consciousness (DOC) are missing, a trial was set up to investigate whether REO is a sign of consciousness or a reflex.
We selected 79 patients out of 150 consecutive patients in our centre with chronic unresponsive wakefulness syndrome (UWS), where the patients are awake but unaware, or patients who were in a minimally conscious state (MCS), during which the patients are awake with reproducible signs of consciousness, with (MCS+) or without (MSC-) language processing. Patients were behaviourally assessed daily for 1 week. We assessed a) the level of consciousness using the Coma Recovery Scale-Revised (CRS-R),4 which is currently considered to be the most accurate clinical measure of consciousness in patients with chronic DOC, b) the presence of REO, and c) the number of times that REO was seen in each patient (repeatability).Furthermore, most patients underwent positron emission tomography (PET)-CT scanning to measure cerebral metabolism. Brain images were then compared to healthy controls.5 A few patients also underwent MRI scanning, during which they were instructed to perform mental imagery tasks.
REO was observed in 19 out of 79 patients (Figure 1). There was a significant relationship between the presence of REO and the level of consciousness. There was also a significant relationship between repeatability of REO between patients in UWS, MCS-, and MCS+. Five out of six patients with UWS that showed REO displayed neuroimaging results more compatible with the diagnosis of MCS. This atypical brain metabolism was seen more often in UWS patients with REO than without REO.
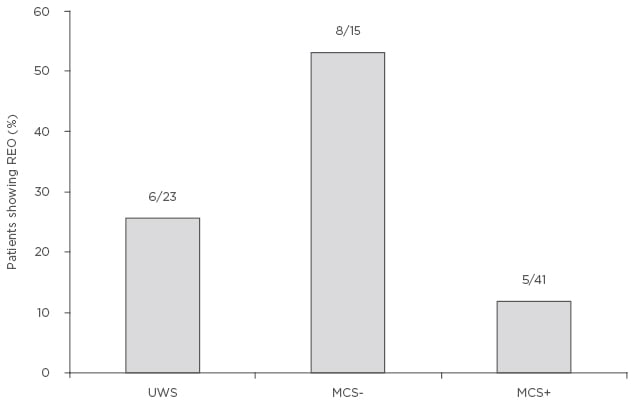
Figure 1: Percentage of unresponsive wakefulness syndrome patients and minimally conscious state patients with and without language processing who showed signs of resistance to eye opening.
MCS+: minimally conscious state with language processing; MCS-: minimally conscious state without language processing; REO: resistance to eye opening; UWS: unresponsive wakefulness syndrome.
In conclusion, in our patient population, REO was observed in one in four patients with chronic DOC. As REO was noted in UWS and MCS patients, identification of REO in a single patient cannot reliably distinguish between voluntary or reflex behaviour. However, at a group level, repeatability of REO was highest in patients in MCS+, suggesting a link between repeatability and the level of consciousness. Our findings therefore suggest a voluntary basis for REO when seen multiple times in a single patient, which stresses the need for multiple assessments in DOC patients.6








