BACKGROUNDS AND AIMS
Anticoagulation and antiplatelet therapy is a widespread management option in various indications, especially in elderly patients who are at greater risk of complications related to any treatment. One of the important and rare complications of anticoagulation and antiplatelet therapy is spontaneous spinal epidural haematoma (SSEH).1,2 Surgery remains the gold standard treatment, especially in cases of progressive neurological deficit.3 In this study, a group of 14 patients with SSEH is presented. Additionally, the clinical symptoms of SSEH, diagnostic procedures, conservative and surgical treatments, and different risk factors are discussed.
METHODS
Between 2010 and 2019, 14 patients (age range: 17–89 years; 10 females) were hospitalised with SSEH in two large hospitals in the Czech Republic. Table 1 presents their demographic and clinical data, including MRI showing haematoma localisation, treatment efficacy, and risk factors with a focus on anticoagulant use. In addition to a detailed clinical neurological examination, the severity of spinal cord disability was assessed using the American Spinal Injury Association (ASIA) Impairment Scale (AIS) classification.
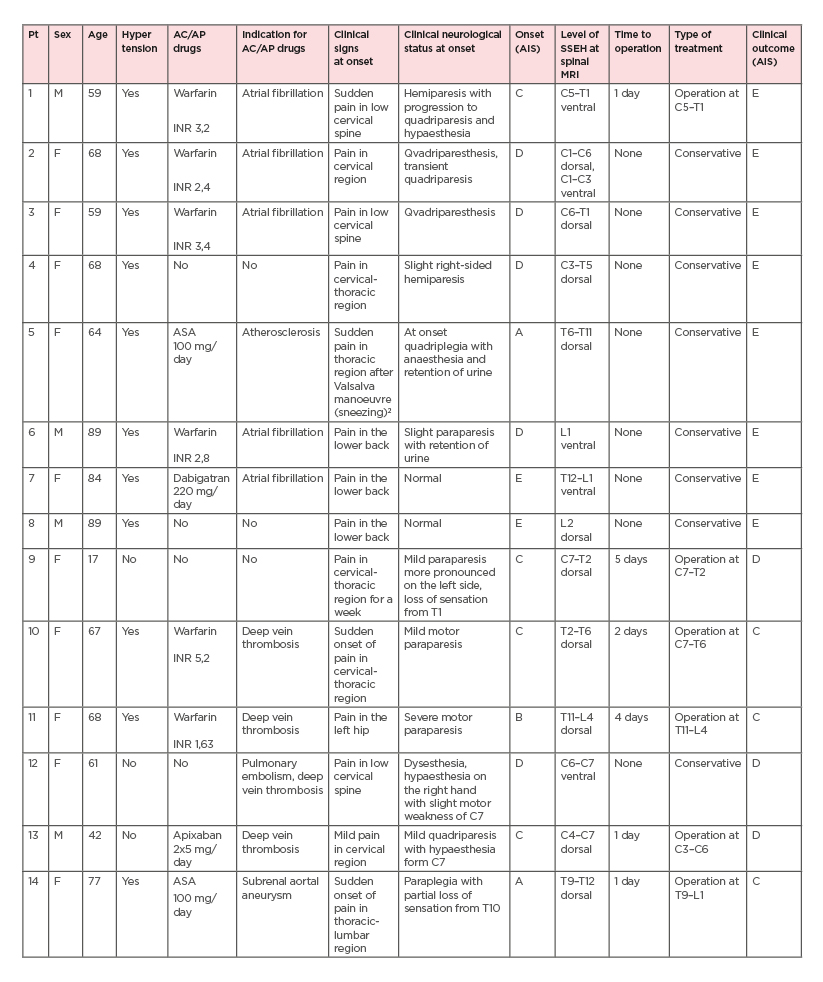
Table 1: Demographic and clinical data of spontaneous spinal epidural haematoma group
Of note, patient 5 developed paraparesis after sneezing,2 clinical improvement to normal status was observed after 24 hours, and patient 9 was pregnant.
AC: anticoagulation; AIS: American Spinal Injury Association (ASIA) Impairment Scale (AIS); AP: antiplatelet; ASA: acetylsalicylic acid; INR: international normalised ratio; pt: patient; SSEH: spontaneous spinal epidural haematoma.
RESULTS
Eight patients received oral anticoagulant therapy (six warfarin, one dabigatran, one apixaban). There was an increase of international normalised ratio values above 3.0 in three patients using warfarin (two cases for atrial fibrillation, one for deep vein thrombosis). Eleven patients experienced arterial hypertension. Two patients were using acetylsalicylic acid of 100 mg/day. In summary, 10 patients out of 14 (71%) were given oral anticoagulant/antiplatelet therapy.
All patients reported acute onset of severe pain as the initial symptom, mostly in the lower cervical spine. Twelve patients reported some degree of neurological deficit accompanying the pain. Only two patients did not develop any neurological deficit. All patients underwent
urgent MRI for the detection of SSEH. With respect to the affected level of the spine, the lower cervical/upper thoracic region was the most common site of involvement (n=7; 50%). Six patients (43%) underwent surgery as a result of rapidly developing spinal cord compression. The clinical conditions of the other eight patients (57%) were more favourable, and conservative approaches were chosen. Ten patients showed clinical improvement by more than one point on AIS classification.
CONCLUSION
SSEH is a rare entity concerning the expansion of blood collection in the spinal canal without clear traumatic or iatrogenic causes, with the prognosis affected by the severity of spinal cord compression, delayed final diagnosis, proper timing in surgical intervention, and well-chosen conservative approach in spontaneously improving cases.3,4 In this study, one of the most important findings was that 71% of patients (mostly in those who were of an older age) received oral anticoagulation/antiplatelet treatment and 57% of patients with slight or mild neurological symptoms were successfully treated with a conservative approach.








