Session Summary
The glomerular disease IgA nephropathy (IgAN) predominately arises in young adults and can progress to chronic kidney disease (CKD) and, ultimately, kidney failure or death. While there are guidelines for treating IgAN, there are still unanswered questions around the condition, including when patients are referred for specialist care, what their health-related quality of life (HRQoL) is, and what other factors may be involved in progression to CKD. These questions were investigated, and findings shown, in three posters presented at the 61st European Renal Association (ERA) Congress in Stockholm, Sweden. The first poster, which surveyed Europe-based physicians who treated at least 50 patients with Stage 1−4 CKD, found that nearly a third of patients were referred to them later than they should have been, given their IgAN symptoms. The survey also revealed that, while over three-quarters of patients were in CKD Stage 3 or above, the majority of physicians (98%) rated a patient’s overall health as good or excellent. In the second poster, both patients and their care-partners (predominantly from Spain and Germany) were surveyed with regard to the humanistic burden of IgAN. In this preliminary analysis of a wider survey, both participant cohorts had a lower HRQoL than a general European population, along with reporting negative work-related impacts of IgAN, and 31% of patients had moderate−severe scores for anxiety and depression. In the third poster, which accompanied an oral presentation, albuminuria was investigated as a factor that may be useful to help ascertain progression and guide IgAN treatment. Utilising data from the Swedish Renal Registry, the authors found that the probability of CKD progression was impacted by albuminuria level, even in cases where this was only slightly above normal. Decreases in albuminuria lowered the hazard ratio for CKD progression. Taken together, these studies show the need to diagnose and treat patients with IgAN on an individualised basis, address both patient and care-partner HRQoL, and consider even those with low-grade albuminuria as at risk of progression.Introduction
IgAN is an immune-complex mediated glomerular disease with an incidence rate of 0.03−10.5/100,000 persons/year.1-3 Although rare, IgAN is the primary cause of glomerulonephritis and is associated with an increased risk of all-cause mortality and a reduction in life expectancy due to kidney failure.4-6 Signs and symptoms of IgAN can vary, but proteinuria is always present. Progression may be slow to rapid, sometimes necessitating aggressive treatment. Patients with IgAN may experience pain and fatigue, along with associated anxiety and depression, all of which can impact their HRQoL.4,7-9 According to 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, treatment options for IgAN include the highest tolerated dose of a renin-angiotensin-aldosterone system inhibitor (RAASi), immunosuppressant therapy (where suitable), and supportive care, such as cardiovascular, blood pressure, and lifestyle management.10
Three posters presented at the 61st ERA Congress in Stockholm set out to address some of the questions that remain about how to best assess an individual patient needs and optimise treatment in those with IgAN. The first, led by Philipp Csomor, utilised real-world data to examine patient characteristics. The second, led by Justyna Szklarzewicz, discussed data from a survey regarding HRQoL of both patients with IgAN and their care-partners. Lastly, Anne-Laure Faucon gave an oral presentation of her group’s investigation into kidney outcomes in patients with IgAN in relationship to albuminuria levels.
Analysis of the Characteristics of Patients with IgA Nephropathy Using Real- World Data from Five European Countries
Philipp Csomor
The first poster11 reported on patient characteristics associated with IgAN through the use of a physician questionnaire and patient chart audit that took place between December 21, 2022–February 6, 2023. The authors proposed that understanding such aspects could help best implement effective, individualised treatment regimens.
The 261 participating physicians were from France, Germany, Spain, Italy, and the UK. Physician inclusion requirements were that they had been in practice between 2−40 years, that they spent more than 40% of their time in a clinical setting, and that they had at least 50 patients with stage 1–4 CKD, with at least four patients who were not on dialysis. Patient chart inclusion requirements were that they had an IgAN diagnosis, were at least 12 years old, were not on dialysis, had an estimated glomerular filtration rate (eGFR) ≥15 mL/min/1.73 m2, and had seen a participating physician within 6 months of the survey date.
Data was collected on 473 patients who were predominantly male (71%) and Caucasian (78%). Of note though, globally, IgAN is most prevalent in people of Asian descent, potentially due to an increased number of risk-associated alleles.12 Age-wise, 2% of patients were <18 years old, 16% were aged between 18–30 years, 38% were 31–49 years, 28% were 50–64 years, and 16% were ≥65 years old. This highlights previous findings that IgAN is predominantly a condition that arises in young to middle-aged adults whose lives may be drastically reduced without proper medical management.7
Twenty-two percent of patients had been referred to their current physician within the past year. This was predominantly by a primary care physician (70%), with 9% referred by another nephrologist, of which almost one-third were referred for specialised care. According to the participating physicians, while 17% of patients were referred early and 54% at an appropriate time, around 26% of patients were referred to them late, and 4% extremely late. Contributing factors to this were reported to be that “the patient remained asymptomatic for a long time,” that there was a “lack of engagement from the patient,” and that “the patient had no regularly scheduled doctor appointments.” Specifically for children, but also applicable to adult patients, KDIGO guidelines recommend that, regardless of whether the disease is active or inactive, patients should be continually followed up, “as they can relapse, even after many years.”10
Patients were divided between those with CKD Stages 1 or 2 (24%), Stages 3a or 3b (57%), or Stage 4 (19%). As can be seen from , at their most recent visit, a physician’s perception of IgAN severity mostly mapped to CKD stage, with, for example, a much higher percentage with CKD4 being perceived as having severe IgAN, patients in CDK3 being rated as mostly moderate for IgAN, and those with CKD1 having mostly mild IgAN. However, CKD stage and IgAN severity ratings were not always concordant. For example, 16% with CKD1 were perceived by their physician as having IgAN that was moderate or severe, and 14% with CKD4 were perceived as having mild IgAN.
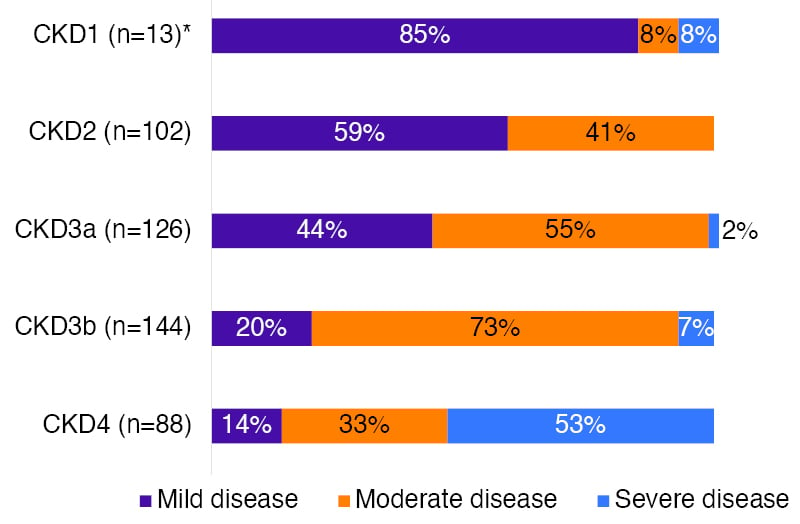
Figure 1: Physicians’ perception of IgA nephropathy severity by chronic kidney disease stage at most recent visit.
*Small number of participants. CKD: chronic kidney disease.
KDIGO guidelines define high risk of IgAN progression as having proteinuria >0.75−1.00 g/day despite ≥90 days’ optimised supportive care.10 In this current survey, 71% of patients had proteinuria >0.5 g/day, and 46% had proteinuria >1.0 g/day (8% had no values available), indicating that many were at risk of progression. Further, while nephrotic syndrome (urine protein >3.5 g/day and low serum albumin) is typically rare in patients with IgAN,10 in this survey, 8% were diagnosed with this condition by a nephrologist.
Most patients (92%) were taking a RAASi, with, on average, patients being prescribed five medications. This number increased in patients ≥50 years old. However, 54% of physicians reported a degree of dissatisfaction with their patients’ response to treatment, although satisfaction levels varied between individual treatment options. This may partly be due to the finding that only two-thirds of physicians felt their patients completely adhered to their treatment regimen.
Fatigue (59%), haematuria (41%), and weight gain (41%) were the IgAN symptoms of mild-to-severe intensity reported with the greatest frequency. Comorbid conditions were common, with 54% of patients having hypertension, 22% hyperlipidaemia, 17% obesity, 15% Type 2 diabetes, and 7% peripheral oedema. These figures reflect findings in larger IgAN studies.7
Despite all these findings, one of the key unexpected results in this study was that physicians rated their patient’s overall health as predominantly excellent (56%) or good (42%), with only 2% rating it as poor. The authors discussed how this revealed a “potential gap in physicians’ perceptions of a patient’s health and their risk of progression to kidney failure.”
Taken together, the authors concluded that the findings of this survey indicate “an unmet need for early diagnosis and treatment of IgAN to ensure that patients receive appropriate, individualised care.”
Humanistic Burden of Immunoglobulin A Nephropathy and Focal Segmental Glomerulosclerosis on Patients and Care-Partners (HONUS): Results for Europe
Justyna Szklarzewicz
The second poster13 reported the burden of Ig A nephropathy and focal segmental glomerulosclerosis on patients and care-partners. Proteinuric kidney disease is associated with both clinical and economic burdens, including high healthcare costs.14 To better understand both patient and care-partner burdens associated with IgAN, an ongoing multi-national, cross-sectional survey, ‘Humanistic burden of rare nephrotic diseases: understanding of the impact of focal segmental glomerulosclerosis and IgAN on patients and care-partners study (HONUS)’, is taking place across Europe and the USA.
In this poster, preliminary results presented included patients with a physician-provided diagnosis of IgAN (confirmed by renal biopsy). Patients were aged ≥18 years and were from Spain (n=16), Germany (n=8), France (n=1), and the UK (n=1). They participated in HONUS from January–October 2023. Participants were excluded if they were participating in a kidney disease clinical trial that included potential active treatment at time of enrolment, or had a history of malignancy, co-existing glomerular disease, or secondary IgAN. While patients with focal segmental glomerulosclerosis were also included in this poster, numbers were low, so the authors focus only on IgAN here.
Presented data included 26 patients with a mean age 42.2 years (standard deviation [SD]: 11.6); 61.5% of which were female. The mean time from diagnosis was 9.6 (SD: 8.6) years. Patients were fairly evenly distributed across CKD stages, ranging from Stages 1−2 (13.0%), 3−4 (26.9%), and 5 with dialysis (15.4%). Additionally, 26.9% were transplant recipients, and 7.7% had unknown status. Also surveyed were 22 care-partners with a mean age of 46.6 years (SD: 9.5). Of these, 59.1% were male and 81.8% were the patient’s life partner.
As previously mentioned, IgAN typically starts in young to mid-adulthood so it encompasses a period of life that greatly includes personal and professional development.7 As such, assessing aspects that may impact these factors is vital. Data from this study showed that patients with IgAN experienced impaired HRQoL in several domains. In general, in European populations, mean 12-Item Short Form Survey15 physical component scores (PCS) and mental component scores (MCS) are on average 50.0 for each score.16 Here, mean PCS was 47.3 (SD: 11.6) (median: 51.6) and mean MCS was 43.2 (SD: 10.9) (median: 44.6), indicating a negative impact on overall HRQoL in comparison to the general European population. For care-partners, figures were 53.3 (SD: 8.8) (median: 55.9) for PCS and 47.9 (SD: 10.8) (median: 50.9) for MCS, indicating a potential impact on mental health aspects of HRQoL. These results were similar to those of the 96 USA adult patients with IgAN and their care-partners also taking part in the HONUS study. In the USA patients, mean PCS and MCS scores were 46.8 (SD: 7.9) and 41.9 (SD: 9.1), respectively, with respective care-partner scores of 50.8 (SD: 7.1) for PCS, and 43.8 (SD 10.2) for MCS.17 Taken together, these confirm previous findings about the impact of IgAN on HRQoL.8
Use of the Generalized Anxiety Disorder Assessment-7 measure18 showed that 30.8% of patients and 9.2% of care-partners had moderate-to-severe anxiety scores (Figure 2). In the USA component of the HONUS study, while a similar 29.1% of patients had moderate-to-severe anxiety scores, moderate anxiety scores were seen to be higher in 13.5% of care-partners (no severe scores).17 This is an important aspect of IgAN to address, as a recent, global, longitudinal survey found that anxiety scores may change little over time in patients with primary glomerular diseases, including IgAN.19
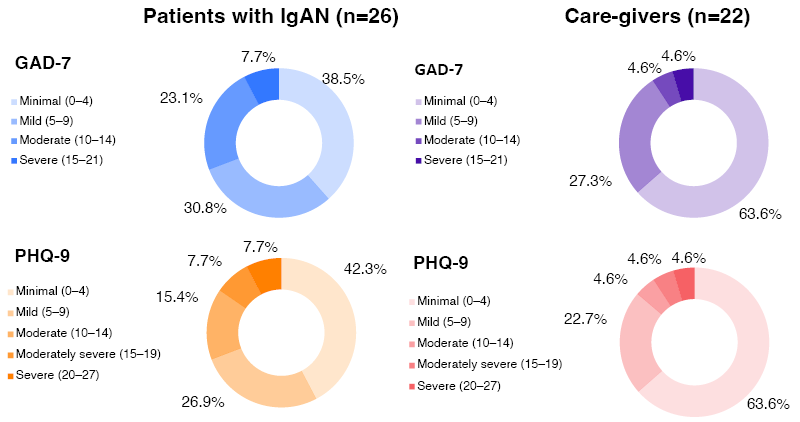
Figure 2: Anxiety and depression scores in patients with IgA nephropathy and their care-partners:
results for Europe.
GAD-7: generalised anxiety disorder assessment-7; IgAN: IgA nephropathy; PHQ-9: patient health questionnaire-9.
Depression scores in this analysis, assessed using the Patient Health Questionnaire-9,20 were moderate-to-severe for 30.8% of patients and 13.8% of care-partners. A higher percentage of both patients (54.1%, of which 51.0% were moderate) and caregivers (40.6%) had moderate-to-severe depression scores in the USA analysis.15 Compared to healthy controls, previous studies have also found higher depression scores in people with glomerular diseases including IgAN.8
Among the 69.2% of patients with IgAN who were employed, findings from the work productivity and activity impairment survey21 showed that over a 7-day period, mean percentage for impairment while working (presenteeism) was 17.7%, with mean percentage for work time missed (absenteeism) being 13.3%. Percentages of activity impairment and overall work impairment for IgAN-related reasons were 27.3% and 17.7%, respectively. In the USA HONUS study, presenteeism percentage was higher, at 25.4%, with absenteeism slightly lower, at 8.2%. For IgAN-related reasons, both activity impairment (34.0%) and overall work impairment (29.8%) were rated as higher.17
For the 86.4% employed IgAN care-partners, mean percent presenteeism was 9.3% and absenteeism was 14.2%. IgAN-related activity impairment was 18.6%, and overall work impairment due to IgAN-related reasons was 9.9%. Corresponding USA figures were mostly higher for care-partners, with 24.7% for presenteeism, 28.8% for activity impairment, and 29.9% for overall work impairment. Absenteeism was lower, at 8.8%.17 Together with the patient figures, these highlight the large burden that IgAN can have on the impacted patient and caregiver’s work and career.
The authors concluded that, at least in these European countries, having IgAN, as well as caring for someone with IgAN, impaired HRQoL, and was associated with anxiety, depression, and impaired productivity. However, the authors noted that scores may have been influenced by the COVID-19 pandemic.
Albuminuria and Subsequent Risk of Kidney Events in Patients With IgA Nephropathy: A Nationwide Cohort Study
Anne-Laure Faucon
The third poster22 discussed albuminuria and the risk of kidney events in patients with IgA nephropathy. Proteinuria levels are one of the main factors KDIGO guidelines use for medical management of IgAN.10 However, some patients with below-target proteinuria can still progress to CKD.6,24 Albuminuria specifically may play a role in IgAN progression, with one meta-analysis of a general population with CKD showing that increase in urinary albumin-to-creatinine ratio (uACR) was associated with progression to end-stage kidney disease.25 With this in mind, this study aimed to “evaluate the risk of CKD progression across the spectrum of uACR.”
This poster, presented orally by Faucon, detailed findings from a cohort of 1,269 patients from the Swedish Renal Registry (taken from 2006–2021) with biopsy-proven, primary IgAN. They comprised 74% men, were a median of 53 years old, and had a mean eGFR of 33 mL/min/1.73 m². Despite the KDIGO guidelines recommendation to treat all patients with IgAN with a RAASi,10 one-fifth were not prescribed such treatment.
“In the first part of the study, we analysed the impact of baseline albuminuria on the risk of CKD progression,” explained Faucon. In these patients, baseline median uACR was 0.7 g/g, with 38% having a uACR >1.0 g/g. Over a median follow-up of 5.5 years, 517 kidney replacement therapy events occurred, 528 patients had an eGFR decline >30%, and there were 667 major adverse kidney events (MAKE, a composite score). According to Faucon, as seen in Figure 3, there was “a strong and incremental association between the level of albuminuria and the risk of CKD progression.” It was of note that substantial CKD progression risk was not just in patients with high albuminuria levels, but also in patients with uACR 0.3−1.0 g/g. “This population,” noted Faucon, “is currently considered at a low risk [for progression].”
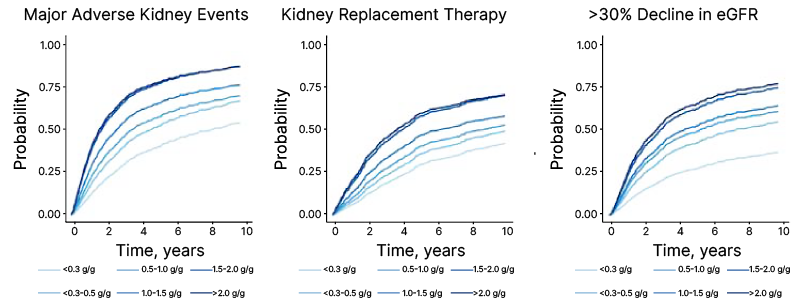
Figure 3: Probability of experiencing major adverse kidney events, kidney replacement therapy, and a >30% decline in estimated glomerular filtration rate over time, according to urinary albumin-to-creatinine ratio.
eGFR: estimated glomerular filtration rate.
In the second part of this study, the authors analysed the impact of 1-year change in uACR in 785 patients who had repeat uACR measurements. Compared to patients with a stable uACR, a 2-fold uACR increase led to hazard ratios (HR) of 1.75 (95% CI: 1.31−2.33) for MAKE, 2.56 (95% CI: 1.79−3.65) for kidney replacement therapy, and 1.18 (95% CI: 0.87−1.60) for >30% decline in eGFR. Conversely, where uACR had a 2-fold decrease, respective HRs were 0.47 (95% CI: 0.36−0.62), 0.49 (95% CI: 0.36−0.68), and 0.49 (95% CI: 0.37−0.65). The latter HR is particularly important as, according to KDIGO guidelines, >30% decline in albuminuria levels is ‘predictive of protection from progression to kidney failure’.10
“Regardless of baseline uACR,” emphasised Faucon, “any reduction in albuminuria was associated with better kidney outcome.” Combined with indications of poorer kidney outcomes even with microalbuminuria, Faucon concluded that “this study suggests that we should optimise clinical and pharmaceutical management in patients with IgAN to decrease albuminuria and delay the risk of CKD progression.”
Conclusion
Taken together, these findings suggest that patients with IgAN should be diagnosed and treated early, with albuminuria taken into account, as substantial CKD progression risk can be observed even in patients with uACR <1.0 g/g. This will help provide individualised, monitored treatment regimens that can negate or slow progress to aberrant kidney outcomes. HRQoL is also a factor that needs to be addressed for patients with IgAN, as well as for their care-partners, as the burden can be considerable.







