Abstract
Chronic kidney disease patients on maintenance dialysis (CKD 5D) experience major morbidity and mortality. No data on survival in Maltese dialysis patients exist; therefore, the aim of this study was to rigorously examine survival statistics in a complete cohort of Maltese CKD 5D patients.
The study population was comprised of all incident chronic patients (N=328) starting dialysis at the renal unit, Mater Dei hospital, Msida, Malta, for 4 consecutive years (2009–2012). Each yearly cohort was analysed in detail up to 31st December 2017, providing up to 8 years follow-up. Demographics (male 65%; female 35%), aetiology of renal failure (diabetic kidney disease: n=191; 58.2%), comorbidities, transplant status, and death were documented. Data collection and follow up were completed and statistical analysis was performed on the aggregated cohorts with SPSS version 23 with censoring up to 31st December 2017.
The cumulative adjusted 5-year overall survival in Maltese CKD 5D patients was 0.36 and 0.25 at 8 years. No statistical difference was observed according to the year of starting dialysis. Cox regression analysis showed that age and transplant status influenced survival. The unadjusted hazard of death increased by 3% for every 1-year increase in age and was increased by 7% if the patient did not receive a transplant, and overall 22% (n=72) of the entire cohort eventually received transplants.
This study reports an approximate 65% mortality at 5 years in Maltese haemodialysis patients, a poor prognosis that, despite optimal medical management, is consistent with worldwide reports.
INTRODUCTION
Chronic kidney disease (CKD) requiring dialysis carries a significantly high mortality rate.1To date there have been no studies in the Maltese islands that have described the incidence and mortality of patients requiring renal replacement therapy (RRT). In this 8-year study, the survival of patients suffering from CKD-5D (estimated glomerular filtration rate [eGFR] <15mL/min/1.73m2) requiring RRT was measured. All incident dialysis cases of CKD requiring dialysis were initially reviewed at a single clinical centre providing a complete source of data for the Maltese archipelago.
Aims
To create an electronic register containing details and comorbidities of Maltese patients who started dialysis in view of CKD-stage 5D between 1stJanuary 2009 and 31stDecember 2012 at the renal unit, Mater Dei Hospital.
To note the survival duration, comorbidities, demographics, and transplant status of patients in the register.
To follow up survival outcomes till the 31stJanuary 2017.
To determine survival outcomes and mortality indicators for patients on RRT, including renal transplant recipients.
Ethics Approval
Permission was granted by the clinical chairman, central executive officer, data protection officer, and consultant nephrologists at Mater Dei Hospital; the Department of Health Information Research (DHIR); and the Faculty Research Ethics Committee, University of Malta (FREC). Patient consent was deemed unnecessary by the FREC as data was gathered from secondary sources and interpreted in a nonidentifiable manner.
Manual records kept at the renal unit, Mater Dei Hospital, detailing information on name, identification number, and date of start dialysis from the 1stJanuary 2008 to the 31stDecember 2012 were reviewed and transferred to an electronic medium (Microsoft® Excel 2007, Redmond, Washington, USA). Information on demographics, age of start dialysis, duration of dialysis, comorbidities, transplant status, aetiology of renal failure, cause of death, and survival were gathered from hospital electronic and manual records (Isoft Clinical Manager®, Sydney, Australia; Electronic Case Summaries) and DHIR databases. Electronic records for the year 2008 were incomplete as they were not yet established. The final data set contained nonidentifiable data.
MATERIALS AND METHODS
Methodology of data collection and interpretation were reviewed by a consultant nephrologist, statistician, and trainee in general practice. A pilot study was carried out involving ten patients from each year reviewing survival from 1stJanuary 2009 to 31stDecember 2012. Criteria for inclusion and exclusion were modified accordingly. The eGFR was calculated using the ‘Modification of Diet in Renal Disease’ formula.
Inclusion criteria:
Starting dialysis between 1stJanuary 2009 and 31stJanuary 2012 or receiving a new kidney transplant.
Maltese national.
History of prior CKD stage 5 (eGFR ≤15mL/min/1.73m2>3 months)
Exclusion criteria:
Starting dialysis outside the timeframe of 1stJanuary 2009 and 31stJanuary 2012.
Prior history of transplantation before starting dialysis.
Foreign national.
Acute kidney injury requiring dialysis eGFR >15mL/min/1.73m2
Defining Renal Replacement Therapy Start Date
Survival figures were taken from the first day of RRT with dialysis or pre-emptive transplant.
Sample Size
At the renal unit, Mater Dei Hospital, 613 patients were started on dialysis from 1stJanuary 2009 to 31stJanuary 2012. Of these patients, 328 cases fitted the inclusion criteria for the study.
Statistical Methods
The age-adjusted survival probabilities (with 95% confidence intervals [CI]) of all incident end-stage renal disease patients receiving RRT and patients receiving a first transplant between 1stJanuary 2009 and 31stDecember 2012 were calculated using the Kaplan-Meier method. However, this method can only investigate the effect of a single categorical confounding factor on survival duration. In order to adjust for several continuous and categorical confounding factors, the proportional hazards Cox regression model was used.
From the electronic case summaries, 60 explanatory variables were identified as possible predictors of the survival duration of renal patients. To identify the significant predictors of survival duration a Cox regression model was fitted using a forward Wald procedure. The parsimonious model identified nine significant predictors which included for example the age of the patient and transplant status (Table 1).
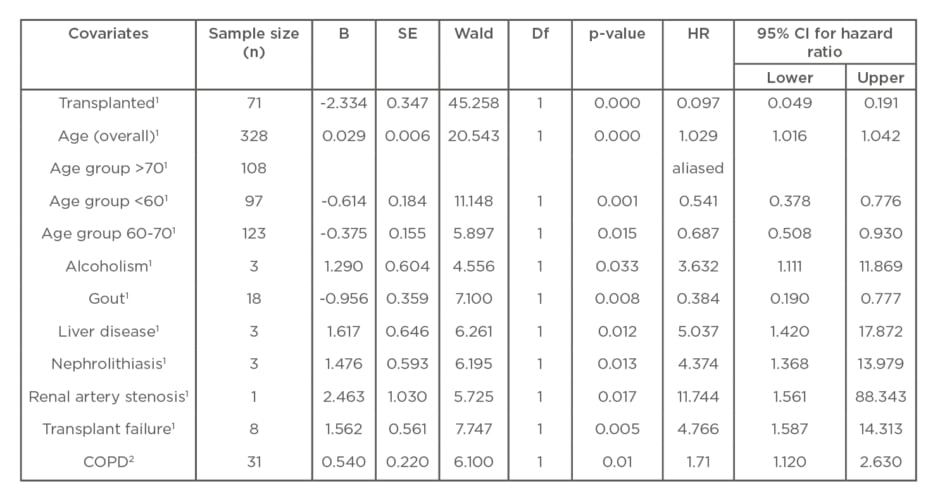
Table 1: Cox regression analysis of hazard ratios and 95% confidence interval for renal replacement therapy: Specific subgroups adjusted to age.
B: constant coefficient; COPD: chronic obstructive pulmonary disease; Df: degrees of freedom; HR: hazard ratio; SE: standard error.
For each covariate the model provides a hazard ratio (HR), which is the ratio of the hazard rates corresponding to the conditions described by two categories of the covariate. Age was adjusted initially to <60 years (n=109), 60–70 years of age (n=97), 71–95 years (n=122), and then in a second analysis at 40 years of age: <40 years (n=28); >40 years (n=300). Multivariate logistic regression analysis was performed to identify independent predictors of mortality which revealed seven factors that did not show variation in responses. A 95% confidence level was used when computing CI and a 0.05 level of significance was used when conducting statistical tests.
Patients were followed up to 31stDecember 2017 providing an 8-year time frame. For the analysis of patient survival on RRT, the first day of RRT was taken as the starting point and the event studied was death. Adjustments were made for age, sex, cause of renal failure, transplant status, and confounding variables on mortality (Table 1). SPSS version 25 was used for statistical analysis.
Methodology for Unadjusted Yearly Incidences per Million Population Rates of Dialysis Dependent Chronic Kidney Disease Based on the Maltese Population
Data on the number of the Maltese population was gathered from the National Statistics Office (NSO) website and the unadjusted incident yearly incidence rate of CKD requiring dialysis per million population (pmp) was calculated (number of incident dialysis patients ÷ total population × 1,000,000).2
End of year population estimates for the Maltese population were; 2009: 395,075; 2010: 395,850; 2011: 397,244; 2012: 398,898.2
Methodology for Incident Patient Survival and Censoring
The dialysis patient population included all patients who started dialysis between 1stJanuary 2009 and 31stDecember 2017. Patients who undertook or attempted a renal transplant were not censored from the study and the 4-year incident data was combined (2009–2012). Measured outcomes were mortality at 1 month, 1 year after 1 month, 5 years, and 8 years after starting dialysis. Data was adjusted according to age (<60 years: n=108; 32.9%, 60–70 years: n=29.6%, >70years: n=123; 37.5%) and gender did not influence survival outcomes in this group.
Methodology of Median Life Expectancy
Several Cox regression models were fitted to relate survival probabilities to dialysis duration for different age groups (<60 years, 60-70 years, >70 age group) for incident patients starting RRT from 2009–2012. The patient inclusion criteria are the same as those of the incident patient cohort described above. Patients were followed until death and those who survived till the end of the study period were right censored. Median life expectancy is the age when the survival function reaches a survival probability of 0.5.
RESULTS
Demographics
The mean age of patients starting RRT was 63.6 ranging from 19 to 91 years. Of these patients, 58.2% cases had diabetes as their primary renal diagnosis (n=191). The majority of patients starting RRT were men (65.2%; n=214) with an average age of 63, of which 56.5% (n=121) were diabetic (Table 2). Causes of renal failure included: diabetes (58.2%); unknown (20.4%); polycystic kidney disease (PCKD) (6.7%); and other (17.6%).
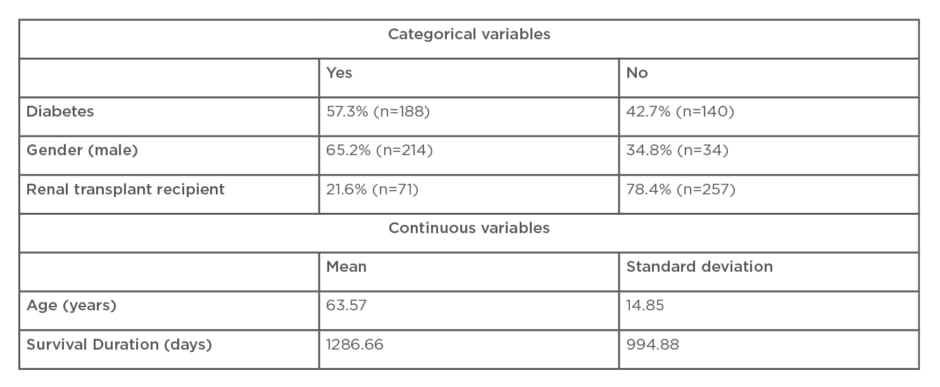
Table 2: Baseline characteristics.
Other included: focal segmental glomerulosclerosis: n=22; obstructive uropathy: n=13; urinary tract infections: n=3; chronic lymphocytic leukaemia infiltration: n=1; IgA nephropathy: n=3; membranous glomerulonephritis: n=2; microscopic polyangiitis: n=1; multiple myeloma: n=3; hypertension: n=1; unspecified glomerulonephritis: n=3; lupus nephritis: n=3; and unspecified vasculitis: n=3.
Incidence (New Renal Replacement Therapy) Rates per Year
The unadjusted yearly incidences pmp rates based on the Maltese population were:2
2009 (n=90): 228 pmp.
2010 (n=84): 212 pmp.
2011 (n=72): 181 pmp.
2012 (n=82): 206 pmp.
Across the 4 years, there were on average two males for every female requiring dialysis.The Chi square test showed that these percentages (65.2% for males and 34.8% for females) vary marginally between the age groups because the p-value (0.213) exceeds the 0.05 level of significance.
Incidence of Renal Transplants per Year
The unadjusted incident renal transplant rates pmp years rates were:2
2009 (n=24): 61 pmp.
2010 (n=15): 38 pmp.
2011 (n=20): 50 pmp.
2012 (n=12): 30 pmp.
Overall the average rate of transplantation for the Maltese population was 44.75 pmp over the 4-year period totalling 71 transplants.
Overall Survival
The unadjusted survival rates following start of RRT was 94% (standard error 0.013) at 1 month; 72% (standard error 0.025) at 1 year after 1 month; 36% (standard error 0.027) at 5 years; and 25% at 8 years (standard error 0.028). At the end of the study almost 70% of the cohort passed away, 21% were transplanted, and 11% remained on dialysis (Figure 1).
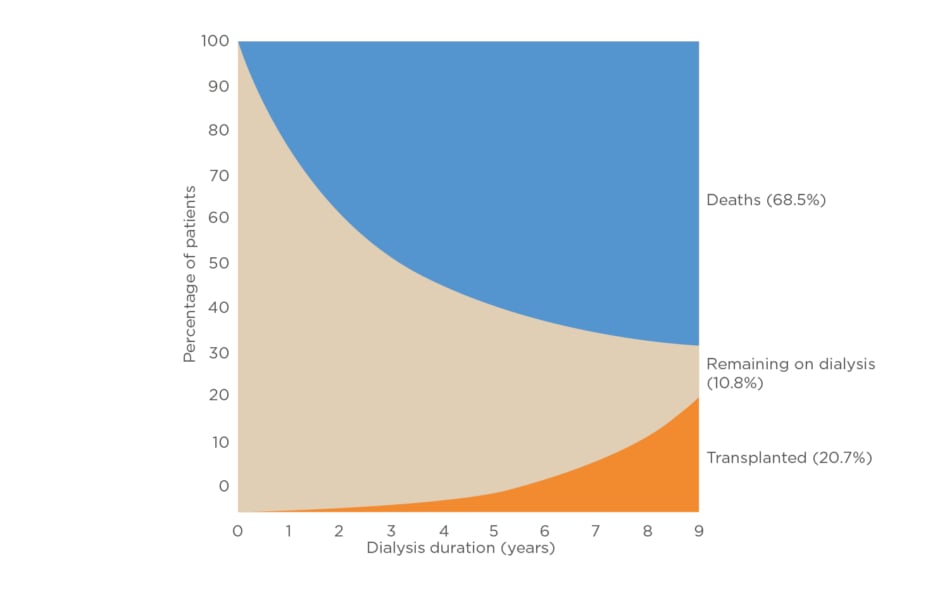
Figure 1: Adjusted cumulative incidence of death and receiving a kidney transplant according to age: incident dialysis patients from Day 1.
Median Life Expectancy
In the >70 age group, 50% of the patients starting RRT survived 1,040 days (2.84 years). Median life expectancy for the 60–70 age group was 1,450 days (3.96 years), whereas for the <60-year age group this was 1,850 days (5.06 years).
Covariates Influencing Survival
Seventy-two variables were included into the Cox regression model. On comparing covariates age, transplant status (p<0.001, 95% CI: 0.049–0.191), transplant failure (p=0.005, 95% CI: 1.59–14.31), nephrolithiasis (p=0.013, 95% CI: 1.37–13.98), renal artery stenosis (p=0.017; 95% CI: 1.56–88.34), gout (p=0.008; 95% CI: 0.19–0.78), liver disease (p=0.012; 95%: 1.42–17.87), and alcoholism (p=0.033; 95% CI: 1.11–11.87) influenced survival (Table 1). On adjusting survival to age 40, chronic obstructive pulmonary disease (p=0.014; 95% CI: 1.12–2.63) was also significant (Table 1).
Age and Hazard of Death
Cox regression analysis demonstrated that for every 1 year increase, the hazard of death increased by 3% (p<0.0001%; 95% CI: 1.016–1.042) (Table 1).
Hazard Ratio According to Year of Dialysis
The HR varies marginally from 1, indicating that the hazard of death is not changing significantly throughout the 4 years.
Survival by Gender
The log-rank test showed that the survival probability functions did not vary significantly between the two genders (χ2=0.018; degrees of freedom (df)=1; p=0.894).
DISCUSSION
The Maltese population has a high incidence of dialysis when compared to other countries in the European Renal Association – European Dialysis and Transplant Association (ERA-EDTA) registry 2012 annual report, with unadjusted rates of dialysis surpassed only by Greece (210.0 pmp) and Portugal (220.0 pmp), reflecting a higher trend for southern European countries.1Rates of incident dialysis cases remained relatively stable over the 4 years. Compared to the average unadjusted transplant rates in Europe, Malta’s annual rates (30.0 pmp) were slightly above average (28.2 pmp), and comparable to Slovenia (30.6 pmp) and Poland (30.3 pmp).1
The overall increase in the hazard of death by 3% (HR: 1.03), and the hazard of death for a patient who received a kidney transplant is 0.097 times the hazard of a patient not receiving a kidney transplant. This implies that the hazard of death for a patient not receiving a kidney transplant is 10.31 times that of a patient receiving a kidney transplant. This result does not eliminate the bias of eligibility for renal transplantation. Wolfe et al.,3established that eligibility for renal transplantation confers a 50% reduced risk of death; however, this study has shown that transplant failure confers an increased risk of mortality as well.
European data has identified an increase in PCKD requiring RRT, attributable to a decrease in cardiovascular mortality in this group of patients. In the Maltese population, PCKD was classified as the second most common cause of end-stage kidney disease requiring RRT, while in European data PCKD ranks fourth.4This may be attributable to a significant proportion (24%) of cases for which the cause remains unknown. Chronic obstructive pulmonary disease has shown reproducibility as a factor that increases mortality in patients with advanced kidney disease.5,6
Diabetic nephropathy has been identified as the number one cause of end-stage kidney disease in Europe.1The latter has also been implicated as the major contributor to CKD requiring dialysis in this study. Malta has a predominantly overweight population with a 10% national prevalence of diabetes.7,8Interestingly, diabetes did not influence mortality in this cohort possibly due to relatively small numbers, although this has been established in other studies.9,10
The emergence of gout as a protective marker (HR: 0.34; 95% CI: 0.19–0.78) may reflect better nutritional status in these patients, but since neither serum albumin nor anthropometric data were studied, this observation could just be a statistical aberration. Gout is associated with a higher cardiovascular risk in the general population; however, further studies are needed.11,12,13
LIMITATIONS
Limitations included BMI, smoking status, socio-economic status, and biomarkers that influence survival and treatment which were not included in the regression analysis. Seven comorbidities were not included in the regression analysis in view of lack of variability. Data was collected from secondary sources and was not adjusted to RRT modality (haemodialysis versus peritoneal dialysis). Cause of death was not included due to variability in reporting.
CONCLUSION
Malta had the third highest unadjusted incident rate of dialysis dependent CKD compared to other European Union (EU) countries in 2012. The largest contributor leading to dialysis is diabetes and should be the focus of prevention and management. CKD requiring RRT incident rates appeared stable with 22% of the cases receiving a transplant. Renal transplant rates were comparable to the EU average in 2012 but on the decrease in trend. Although transplantation is associated with increased survival it is accompanied by an increased mortality when failure occurs. Diabetes did not appear to influence survival in this group.








