BACKGROUND AND AIMS
Chronic kidney disease (CKD) has been linked with an increased risk of cardiovascular events, especially in the dialysis population. In patients with CKD, heart function disturbances are twice as common as in the general population.1 Heart failure (HF) is a major cause of cardiovascular mortality in patients with CKD.2 Bearing in mind that left ventricular hypertrophy is considered to be one of the most important parameters for the occurrence of cardiovascular disease in CKD,3 the aim of the present study was to evaluate the association of left ventricular diastolic dysfunction with HF in patients with CKD.
MATERIALS AND METHODS
The research was conducted as a prospective observational study, which included 30 patients with CKD, Stages III and IV according to Kidney Disease Improving Global Outcomes (KDIGO) staging,4 and left ventricular diastolic dysfunction. The study also included 30 control subjects who had left ventricular diastolic dysfunction but without CKD. Pulse-wave (PW) Doppler echocardiography in the apical four-chamber view and tissue Doppler imaging were performed to assess left ventricular function.5 The measurements of mitral inflow by PW Doppler covered early (E-wave) and late (A-wave) diastolic feeling velocities, peak early diastolic velocity at the septal (e′septal) and lateral (e′lateral) mitral annular sites, and E/A ratio.
RESULTS
A comparison of left ventricular function parameters between two groups of study participants indicated that left ventricular ejection fraction (0.57±0.05% versus 0.61±0.03%) was statistically reduced in patients with CKD compared to control subjects (p<0.001). Contrary, left ventricular mass index (119.8±27.0 g/m2 versus 100.8±20.4 g/m2; p=0.003) was significantly higher in the patients with CKD (Figure 1A). There were no significant differences in values of left ventricular end-diastolic (53.7±4.6 mm versus 54.2±3.5 mm; p=0.636) and left ventricular end-systolic (34.7±4.5 mm versus 35.7±2.3 mm; p=0.265) dimension between patients with CKD and control subjects. The mitral inflow imaging pointed to more pronounced left ventricular diastolic dysfunction in patients with CKD than in the subjects without CKD; e′septal (p=0.009) and e′lateral (p<0.001) velocity (Figure 1B). E/A ratio showed no marked deviation between the two study groups (p=0.787). On the other hand, when the authors analysed the frequency of HF, it was noted that newly developed episodes of cardiac decompensation were more frequent in patients with CKD than in the control group (Χ2=6.667; p=0.010). Regression analysis confirmed the predictive significance of left ventricular echosonographic characteristics on the occurrence of HF in patients with CKD (odds ratio [OR]: 1.56; 95% confidence interval [CI]: 1.11–2.18; p=0.011) and for left ventricular mass index: (OR: 1.68; 95% CI: 1.01–2.80; p=0.048 for e′).
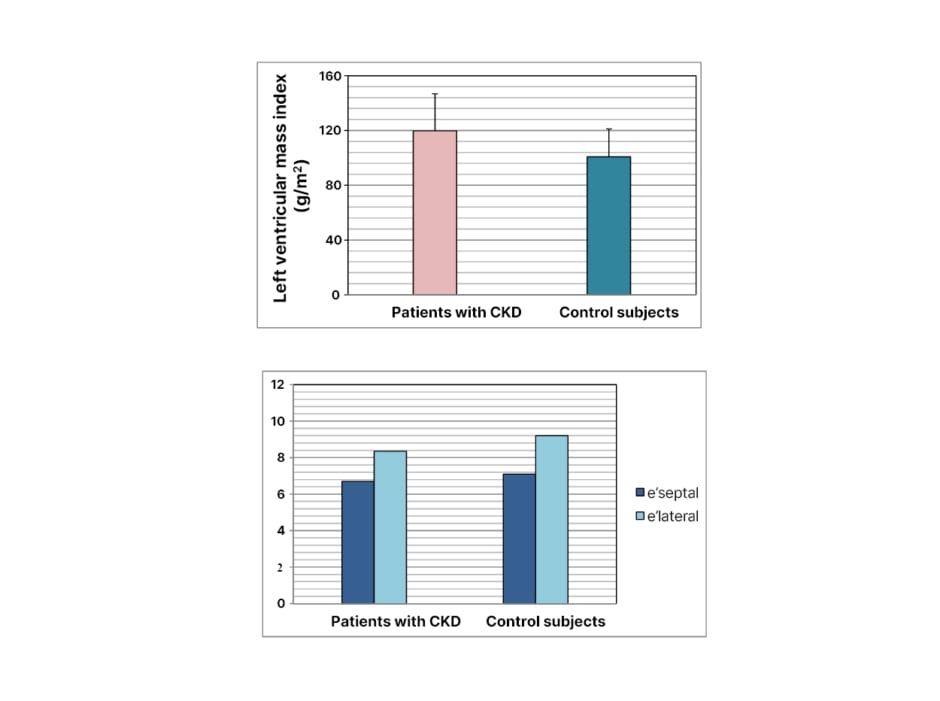
Figure 1: A) Left ventricular mass index and B) left ventricular diastolic dysfunction in patients with CKD and control subjects.
CONCLUSION
HF is more common in patients with CKD than in patients with normal kidney function. There is a positive relationship between the presence of left ventricular diastolic dysfunction and the occurrence of HF in patients with CKD. ●








