INTRODUCTION
Severe COVID-19 infection may result in hypoxaemic respiratory failure, necessitating invasive mechanical ventilation.1-3 The authors revisited the phenomenon of asymptomatic patients despite very low pulse oximetry readings, the so-called ‘sweet hypoxia’, ‘happy hypoxia’, or ‘silent hypoxaemia’.4-6 This abstract review describes, for the first time, the sequential chest radiographic images representing the progressive radiological trajectory of COVID-19 pneumonia.7
CASE REPORT
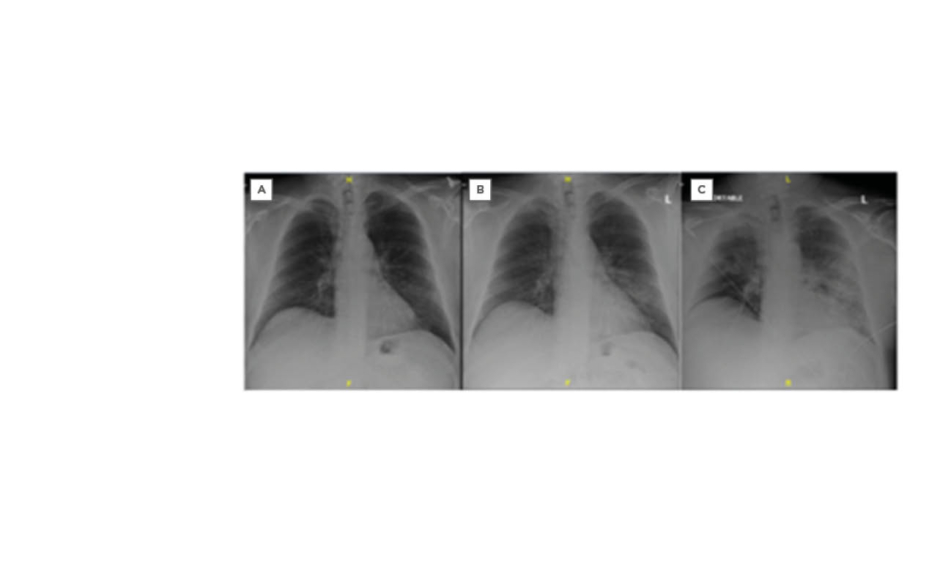
A 62-year-old Caucasian male who was obese, hypertensive, and an ex-smoker, was diagnosed with mild community-acquired pneumonia in mid-March 2020, following evaluation for low-grade fever. He had travelled to Florida and Texas, USA, in the previous month.7 He tested positive for COVID-19 by reverse transcription PCR. One week later he was admitted to a community hospital with a 1-day history of new shortness of breath and loose stools. Chest radiograph revealed new patchy left lower lobe air-space infiltrate (Figure 1B). Treatment included nasal cannula oxygen, intravenous fluids, intravenous azithromycin, and intravenous ceftriaxone. He improved and was discharged the next day on azithromycin (500 mg per day for 3 days) and cefdinir (300 mg twice daily for 5 days).
He was readmitted approximately 18 hours post-discharge with worsening dyspnoea. Chest radiograph showed worsening bilateral infiltrates (Figure 1C) and he soon required emergent intubation in the emergency department (Figure 2A). He was transferred to the intensive care unit on intravenous vancomycin and intravenous cefepime. He developed septic shock and required intravenous norepinephrine. With worsening chest radiographs (Figures 2B and 2C), he was subsequently transferred to a tertiary medical centre. Intravenous azithromycin (500 mg daily) and intravenous ceftriaxone (2 g daily) were administered for 8 days. Chloroquine phosphate (500 mg twice daily) was added. Intravenous norepinephrine was continued. He was extubated after 4 days and discharged home after 9 days, with normalised creatinine of 1.03 mg/dL.7
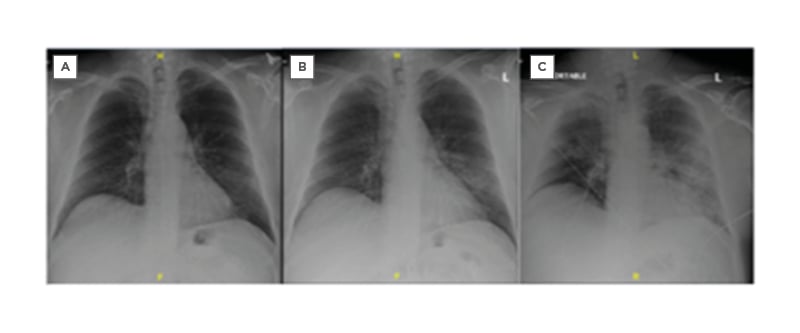
Figure 1: Sequence of chest radiographs. A) Normal in November 2019. B) Before initial hospital admission (20th March 2020, at 2:10:10). C) Just prior to intubation in the emergency department following the second admission (22nd March 2020, at 3:32:01).
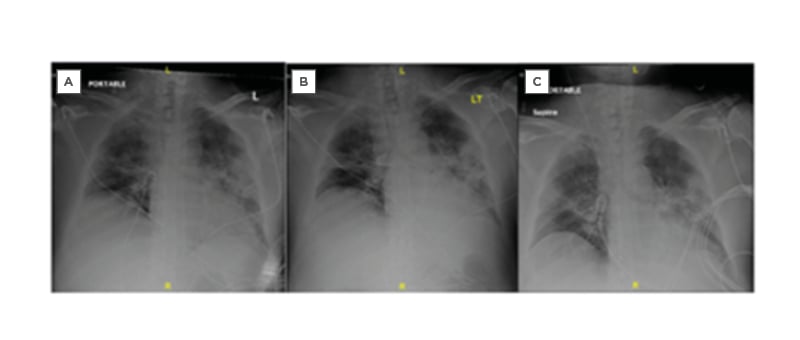
Figure 2: Series of chest radiographs following intubation in the emergency department. A) 22nd March 2020, at 4:27:11. B) Half an hour post-intubation (22nd March 2020, at 5:08:38). C) Approximately 4 hours post-intubation in the intensive care unit before transfer (March 22nd 2020, at 8:10:30).
DICSUSSION AND CONCLUSIONS
The authors have, for the first time, demonstrated in meticulous and real-time details the sequential chest radiographic images of the changes of the progressive radiological trajectory of COVID-19 pneumonia.7 The place of non-invasive ventilation demands further study.8-10 The so-called ‘sweet hypoxia’ or ‘happy hypoxia’ or ‘silent hypoxaemia’ in COVID-19 is revisited; indeed, it is not limited to patients with COVID-19.3,5 The need to mitigate lung barotrauma is mandatory.8-10 Finally, prognostication of pneumonia in COVID-19 is unpredictable.7 Premature discharge from the hospital is strongly discouraged.7