INTRODUCTION
Hereditary nephropathies should be suspected in adults with a family history of chronic renal alterations,1 and children should be screened, particularly in autosomal-dominant diseases.2 However, there are cases of hereditary nephropathies that manifest in childhood (linked to the X chromosome and atypical cases), and from the correct aetiology these cases could be identified in some adults with an erroneous or unknown diagnosis of chronic kidney disease. It could even be possible to discover patients who should be followed up with nephrology consultations.3
OBJECTIVES
The objectives of this study were to analyse patients referred to the nephrology department with hereditary nephropathies diagnosed based on their children in the paediatric nephrology department, and to determine the correct diagnosis of patients with chronic kidney disease not previously identified.
MATERIALS AND METHODS
Paediatric patients in a paediatric nephrology clinic were diagnosed by neonatal screening for cystinuria4 or by a positive genetic study of another aetiology. Adult patients with hereditary nephropathy were then identified following the screening of their children.5 Variables in the study included the age and sex of children and adults with chronic kidney disease, aetiology of the hereditary nephropathy, genetic study, and clinical profile (blood, urine, and renal ultrasound).
RESULTS
The study included 68 children (65% males) aged 0–7 years at diagnosis; 14 were diagnosed following a positive genetic study. After the screening of the paediatric patients, 76 adults (58% males) were identified, with 8 shown to have previously been in follow-up due to undiagnosed chronic kidney disease.
Two different groups were identified: those diagnosed by neonatal screening (62 cystinurias) and those diagnosed via genetic study of their children (1 case of Alport syndrome,6 3 cases of hepatocyte nuclear factor 1β-associated kidney disease,7 1 case of Barakat syndrome, 1 case of autosomal dominant polycystic kidney disease,8 6 cases of Dent disease,9 1 case of PAX2-related disorder, and 1 case of hypophosphataemic rickets linked to the X chromosome [hl]Figure 1[/hl]).
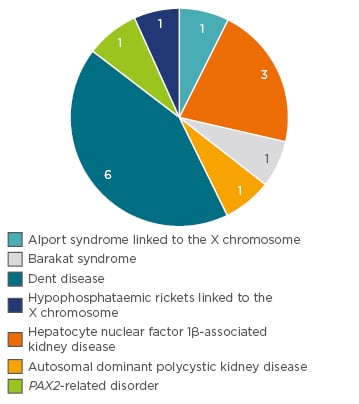
Figure 1: Number of adult patients diagnosed with hereditary nephropathy (not cystinuria) via genetic study.
CONCLUSION
The consultation of paediatric nephrology provides a step towards the improvement of the diagnosis of hereditary nephropathy, especially in cases of undiagnosed chronic kidney disease. As nephrologists, we should suspect these diseases upon the first examination of adult patients.10








