Phthalates can disturb the endocrine system and are reported to have associations with breast cancer.1 Patients with chronic kidney disease (CKD) are known to have a greater risk of urothelial cancer (UC) than the general population.2 Whether it is related to higher phthalate exposure is not known at present and this study was conducted with the aim of answering this question.
This prospective, multicentre, case-control study of UC was initiated by the Taiwan Urothelial Cancer Consortium with the aim of investigating the risk factors of UC with multiple risk domains. Ten hospitals distributed through different regions of Taiwan joined the consortium. These hospitals had diverse healthcare levels, from tertiary settings to local hospitals. Subjects were Taiwanese patients with CKD but without UC (controls) and patients with ongoing UC. The CKD controls were best matched with UC patients from the same living area. For non-UC patients, blood and urine specimens were collected at the time of the structured interview. For UC patients, urine and blood were collected before operations.
The collected urine specimens were stored at -80°C before analysis. With liquid chromatography-electrospray ionisation-tandem mass spectrometry (LC-ESI-MS/MS), we measured seven phthalate metabolites (MBzP, MCHP, MiNP, MMP, MCPP, MiBP, and MEHHP) as biomarkers for exposure to phthalates. MiBP is a urinary metabolite of dibutyl phthalate and MEHHP is a urinary metabolite of di-(2-ethylhexyl) phthalate. A multiple logistic regression analysis was performed to evaluate the association between UC risk and clinical parameters, including log-transformed creatinine-corrected urinary phthalate metabolite concentrations. Odds ratios (OR) and 95% confidence intervals of OR were calculated.
From 2013 to 2017, we recruited 224 UC patients and 272 CKD controls who had adequate urine specimen collections and complete datasets. Five of the metabolites, MBzP, MCHP, MiNP, MMP, and MCPP, were detected in <40% of samples, and were not further analysed for statistical significance. Among UC patients, the median concentration of urinary MEHHP was significantly higher in the UC cohort than in the control group (42.41 µg/g versus 22.03 µg/g, respectively); however, the median concentration of MiBP did not show any difference between groups (9.71 µg/g versus 10.74 µg/g, respectively). The adjusted OR of MEHHP was 1.42 (95% confidence interval: 1.21–1.68; p<0.001) in multivariate logistic regression after adjusting for age, renal function, non-steroidal anti-inflammatory drug use, exposure to environmental toxins, and the use of traditional Chinese medicine. Analysis within MEHHP concentrations showed a dose-response relationship of OR for urothelial cancer UC risk (Figure 1).
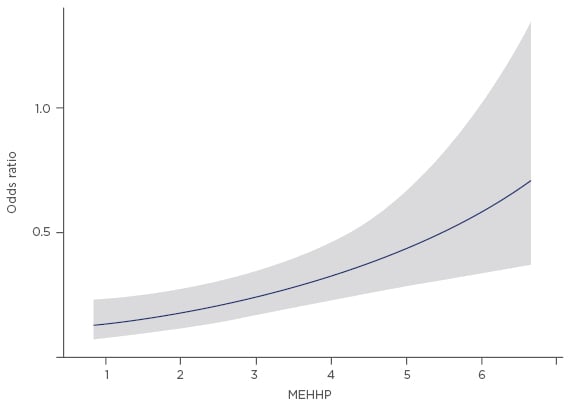
Figure 1: Analysis within urinary MEHHP concentrations (log-transformed) showed a dose-response relationship of odds ratios for urothelial cancer risk.
Previous studies have shown that phthalates promote and induce tumourigenesis in a variety of cell types through aryl hydrocarbon receptor-mediated genomic and non-genomic pathways.3 We speculate the activation of these pathways by phthalates may be related to our observations.
In conclusion, higher urinary concentration of MEHHP is correlated with the increased risk of UC. These findings suggest high environmental exposure to phthalates may contribute to the development of UC in CKD patients. Further studies are needed from other populations with a different range of phthalate exposure to confirm our findings.








