INTRODUCTION
Overhydration (OH) is highly prevalent in haemodialysis (HD) patients1 and is a strong risk factor for mortality.2,3 It has been shown that pleural B lines, also known as pulmonary or pleural comets, appear alongside the presence of extravascular pulmonary fluid. Absent in normal lungs, the resolution of B lines in HD patients seems to occur in real time as the ultrafiltrate (UF) progresses.4 However, it has not been investigated whether this technique has a relationship with the results obtained by bioelectrical impedance analysis (BIA)5,6 in the estimation of OH and if it can be used to estimate the UF to be removed through HD. The study’s main objective was to evaluate the presence of B lines in patients with OH data according to their BIA assessment.
STUDY DESIGN
This study was based on a unicentric transversal observational cohort.
METHODS AND PARTICIPANTS
Hydration status was assessed using BIA and pulmonary ultrasound in 17 patients who received HD for at least 6 months. The inclusion criteria were no amputations, metal prostheses, or pacemakers; an ejection fraction of the left ventricle >50%; and no New York Heart Association (NYHA) Class IV heart failure or any history of cardiovascular or pulmonary decompensation in the last 3 months.
RESULTS
The demographic, clinical, and laboratory data of the participants are described in Table 1. The mean age of the patients was 44.1 years, 76.5% were hypertensive, 41.2% were diabetic, 23.5% presented with oedema of the lower extremities, and 35.3% had jugular engorgement. A normal BMI was measured in 41.2% of the patients and only 4 patients (23.5%) followed the nutritional recommendations.
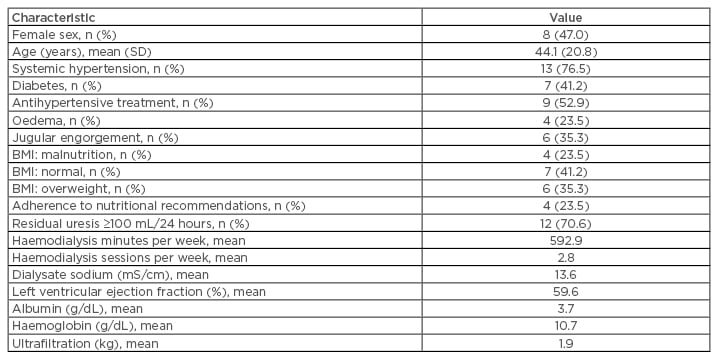
Table 1: Demographic, clinical, and laboratory characteristics of the study participants (N=17).
The patients received an average of 2.82 sessions of HD per week, with equal sodium conductivity in all cases (13.6 mS/cm) and an average UF of 1.94 kg. The average serum sodium level was 134.4 mEq/L (standard deviation: 2.5) and average serum albumin was 3.66 g/dL (standard deviation: 0.4). A positive correlation was found between OH and the number of B lines (r=0.62; r2=0.38; p=0.008). No correlation was found between the dry weight and the number of B lines. The distribution of B-type natriuretic peptide in the sample ranged between 12 and 5,000 pg/mL, with a mean of 1,038.9 pg/mL (standard deviation: 1,448.27), showing a positive correlation with the number of B lines (r=0.70; r2=0.52; p=0.001). Systolic blood pressure also positively correlated with the number of B lines (r=0.71; r2=0.21; p=0.001).
CONCLUSION
Analysis of the data showed that there was a positive correlation between OH measured by BIA, B-type natriuretic peptide, and systolic blood pressure with the number of B lines shown on pulmonary ultrasound. These findings show these methods can be used to estimate OH in HD patients, with the advantages of being affordable and accessible methods that can be performed at the patient’s bedside.








