INTRODUCTION
Euvolaemia is a major issue in chronic kidney disease, as volume overload (VO) is related to cardiac dysfunction, inflammation, and mortality.1 Guidance on how to achieve and maintain euvolaemia in dialysis patients is hampered by the absence of factors associated with VO.2 The aim of this study was to compare volume status between haemodialysis (HD) and peritoneal dialysis (PD) patients and to identify factors associated with hypervolaemia.
METHODS
The study included 47 HD patients and 21 PD prevalent patients. Baseline characteristics and comorbidities were evaluated. For each patient, blood pressure, pro-brain natriuretic peptide (pro-BNP), bioimpedance analysis, and echocardiographic variables were evaluated. In HD patients, the values were recorded pre-session. Overhydration (OH), extracellular water (ECW), and OH/ECW were used as volume indices; an OH/ECW >15% was the cut-off used to define OH.
RESULTS AND DISCUSSION
The characteristics of the population are summarised in Table 1.
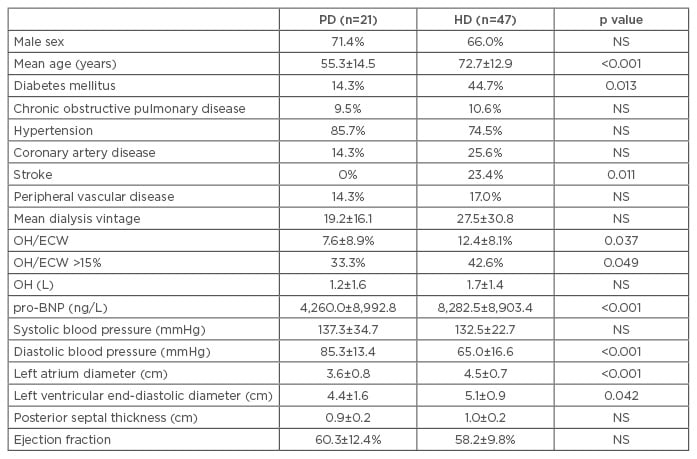
Table 1: Overall characteristics of the population.
OH: overhydration; ECW: extracellular water; pro-BNP: pro-brain natriuretic peptide; HD: haemodialysis; PD: peritoneal dialysis; NS: not significant.
Fluid overload is frequently present in dialysis patients and leads to adverse clinical outcomes; thus, ensuring dialysis patients are euvolaemic is essential.1 Despite the fact that VO is a preventable and treatable condition, managing fluid balance and achieving true dry weight is still a major challenge in both HD and PD patients. However, indices obtained from bioimpedance analysis are useful for the assessment of fluid status. The different dialysis modalities have different effects on fluid volume control. PD is believed to provide better fluid control due to its continuous ultrafiltration and the fact that residual renal function is better preserved.3 The findings of our study corroborate this explanation. Although the HD patients were older and had a higher incidence of diabetes and stroke, they were also more overhydrated compared to PD patients and had higher pro-BNP values and echocardiography measurements, such as left atrial diameter and left ventricular end-diastolic diameter (LVEDD). Overall, 27 of 68 (40%) patients had OH/ECW >15%, and this ratio was positively correlated with pro-BNP (r: 0.79; p<0.001), left atrial diameter (r: 0.64; p=0.002), and LVEDD (r: 0.73; p<0.01). This indicates that fluid overload has an effect not only on cardiac remodelling, but there also seems to be an effect with a well-established cardiovascular laboratory parameter, pro-BNP, indicating that it is not only a marker of cardiac dysfunction but is also associated with VO. There were several independent factors (p<0.05) associated with OH in multivariate logistic regression analysis: higher systolic blood pressure (odds ratio [OR]: 1.05; confidence interval [CI]: 1.01–1.09) and higher LVEDD (OR: 1.99; CI: 1.09–3.06).
CONCLUSION
Excess fluid may lead to adverse events, especially in cardiac conditions. So, finding tools to achieve euvolaemia is of the utmost importance. In this cohort, fluid overload was more common among HD patients, although they were older and had more severe diabetes. Globally, OH was associated with higher pro-BNP, systolic blood pressure, and worse cardiac parameters, especially LVEDD.








