BACKGROUND
Despite clinical and lifestyle advantages of home haemodialysis (HHD) compared to in-centre hemodialysis,1 it remains underutilised in the province of Saskatchewan, Canada. Only 2.5% of patients with end-stage renal disease utilise the modality,2 which is far below that of other developed countries. The aim of the study was to explore the patients’ perception and to identify the barriers to use of HHD in Saskatchewan, Canada.
METHODS
In this cross-sectional study, the authors approached all prevalent in-centre hemodialysis patients across Saskatchewan (two major centres [Regina and Saskatoon] and five associated satellite units attached to each centre) from June 2018 to January 2019. 398 patients agreed to participate in the study. For comparison of responses between main and satellite units, Chi square and Mann–Whitney U test were used, as appropriate.
RESULTS
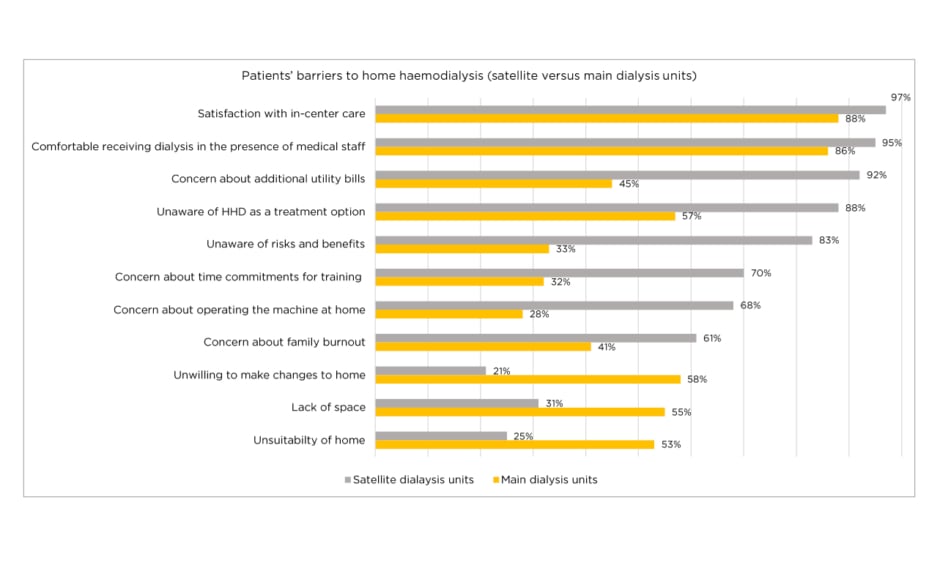
Satisfaction with current dialysis care (91%), increase in utility bills (65%), fear of catastrophic events at home (59%), medicalisation of one’s home (54%), and knowledge deficits towards treatment modalities (54%) were the main barriers to HHD uptake. Compared to patients dialysing in the main units, satellite patients chose not to pursue HHD more frequently because they had greater satisfaction with their current dialysis unit care (97% versus 87%, respectively; p<0.001), felt more comfortable dialysing under the supervision of medical staff (95% versus 86%, respectively; p<0.007), could not afford additional utility costs (92% versus 45%, respectively; p<0.001), were unaware of the risks and benefits of HHD (83% versus 33%, respectively; p<0.001), had concerns over time commitments for training to HHD (69% versus 32%, respectively; p<0.001) and had concern for family burnout (60.8% versus 40.6%, respectively; p<0.001) (Figure 1).
Figure 1: Patients’ barriers to home haemodialysis (satellite versus main dialysis units).
HHD: home haemodialysis.
CONCLUSIONS
Satisfaction with in-centre care; lack of awareness and education, specifically in the satellite population; concerns with family burnout; and expenses associated with utilities and training time will need to be addressed in order to increase the uptake of HHD. With identifying to utilising HHD, it is possible to better design centre-specific programmes to address the unique barriers leading to low utilisation of HHD. The findings will help healthcare decision or policy makers formulate well-informed decisions to address province specific barriers in order to increase the uptake of HHD.
Some of these issues can be addressed as a programme (education), but others will require policy level changes (reimbursement of costs borne by the patient).