Abstract
Background: Although hospital admission is frequently due to the exacerbation of chronic diseases, most often it is caused by an underlying infectious process. Patients often have several admissions per year, making them at risk for recurrent infections, increased morbidity, and the emergence of resistant strains of microorganisms.
Methods: This is a retrospective, descriptive study of all patients with an infectious disease diagnosis, who were admitted to the medical ward of a tertiary hospital during a 5-year period. Information was collected from electronic medical files regarding gender, age, autonomy, comorbidities, primary diagnosis, in-hospital length of stay, and mortality as well as microbiological data surveillance.
Results: A total of 355 patients fulfilled the inclusion criteria. Amongst the sample analysed, the average age was 78.10+12.47 years years. Of the patients, 57.2% (203) were female, with most patients considered as dependent according to Katz score. The average Charlson Comorbidity Index (CCI) score was 6.28+2.74, increasing with age. The main diagnostic categories were respiratory (191 patients: 137 with pneumonia and 49 with acute bronchitis) and urinary tract (138 patients: 69 with pyelonephritis and 66 with cystitis). Urinary tract infections were more frequent in females and in dependent patients. Only 37.8% of infections had a microbiologic isolate: Escherichia coli (28.4%), Pseudomonas aeruginosa (12.7%), and Klebsiella pneumoniae (8.2%). The overall mortality was 6.77%.
Conclusions: The frequent in-hospital admission due to infectious diseases makes it imperative to characterise and follow-up on evolution of the disease itself in order to better know the characteristics of community-acquired diseases, establish routes of transmission and outbreak identification, microbiology patterns, and resistance towards further improving empiric therapy.
INTRODUCTION
A wide variety of infections contribute to acute care admissions to general internal medical units. There is an increasing trend in the burden of infectious disease (ID) hospitalisations, as reflected by an increase in the proportion of hospitalisations attributable to IDs.1 IDs cause widespread morbidity and mortality worldwide. Extensive improvements in sanitation, vaccine development, and other public health measures led to a decrease in the IDs burden. However, IDs hospitalisation rates did not follow the same decrease trend in the rate of all-cause hospitalisations in the last part of the 20th century.1-3
The ongoing changes in the demographics due to an ageing population also pose a challenge to the departments of acute care such as internal medicine. As patients become older, the functional impairment rate and the prevalence of chronic disease increases and, as such, comorbidities (defined by the number of chronic diseases in addition to the index disease)3 and also the susceptibility to IDs increases.
Acute care is defined by the World Health Organization (WHO) as “a range of clinical healthcare functions, including emergency medicine, and others as urgent care, and short-term inpatient stabilisation,”⁴ and comprises the initial assessment, diagnosis, treatment, and discharge or transfer to an appropriate setting of patients.2,5 Worldwide, the absolute number of acute admissions has increased, as have the acute admissions due to IDs, and this increase associated with a higher prevalence of older patients with different characteristics has challenged the structure of acute hospital care.6
The epidemiology of IDs is a composite of several environmental, behavioural, social, and biological variables, including the selective effect of drugs or vaccines, and other unpredictable events that can change over time and have potentially important effects on global health. Throughout the last century, there has been substantial variation in the number of hospitalisations of this disease group, namely respiratory infections, diarrhoeal diseases, HIV or AIDS, tuberculosis, and malaria, although major differences in their ranking exist between high- and low-income countries.7,8
Multiple studies over the past two decades have shown that morbidity and mortality due to IDs are associated with significant health care burdens and expenditures.3,7,9 Apart from having chronic diseases, patients in the departments of internal medicine comprise a complex population, due to the varying degrees of disease severity and functional impairment.9,10
The overall aim is to evaluate the population admitted due to IDs in terms of patient characteristics, admission rates, main reasons for admission, and prognosis after a short-term follow-up, establishing a trend in the admissions due to infectious causes in a tertiary care centre.
METHODS
The authors performed a retrospective study on all patients with an infectious diagnosis who were admitted to an acute ward of a tertiary hospital from 2012 to 2016. Inclusion criteria were an age over 18 years and an International Classification of Diseases, Ninth Revision (ICD-9) code for infectious and parasitic diseases (001–139; 320–326; 420–429, 460–519; 590; 595; 601; 680–686; 730; 995.9; and 996–999).
The authors performed an electronic medical review and collected demographic data, patients’ autonomy assessed by Katz score, comorbidities (by the Charlson Comorbidity Index [CCI]), and primary diagnosis (according to a diagnostic category). They also collected data related to microbiology and antibiotic treatment.
The authors’ outcomes were length of stay, microbiological positivity, antibiotic use and switch, and mortality.
Data were analysed as non-normal, with median and interquartile range. Trends throughout the years were evaluated by linear regression for continuous normal outcomes, tests for trends for continuous non-normal variables, and standard correlation for the binary outcomes. A p-value of <0.05 was considered to be significant. Analysis was conducted with Stata 14 (StataCorp, College Station, Texas, USA).
RESULTS
From January 2012 to December 2016, the authors included a total of 2,615 patients admitted to an acute ward with an infectious diagnosis. An increase following a decrease was observed over the years (p<0.0001). The median age was overall unchanged (80 years [interquartile range: 71–87 years]; p=0.5000). However, the male prevalence decreased from 53% to 43% (p<0.0001), and a peak was observed for the CCI (p=0.0010) in 2015 (Table 1).
The major diagnostic criteria were respiratory (34.0%), genitourinary (34.0%), gastrointestinal (4.0%), soft tissue (4.0%), systemic (3.0%), bone and joint (0.7%), and central nervous system (0.3%). There was a trend towards a decrease in respiratory infections, along with an increase in genitourinary infections (p<0.0001 Table 1). The most frequent diagnoses were respiratory and genitourinary and followed the same trend (p=0.0080): pneumonia (38%), cystitis (18%), pyelonephritis (16%), and bronchitis (15%) (Table 1).
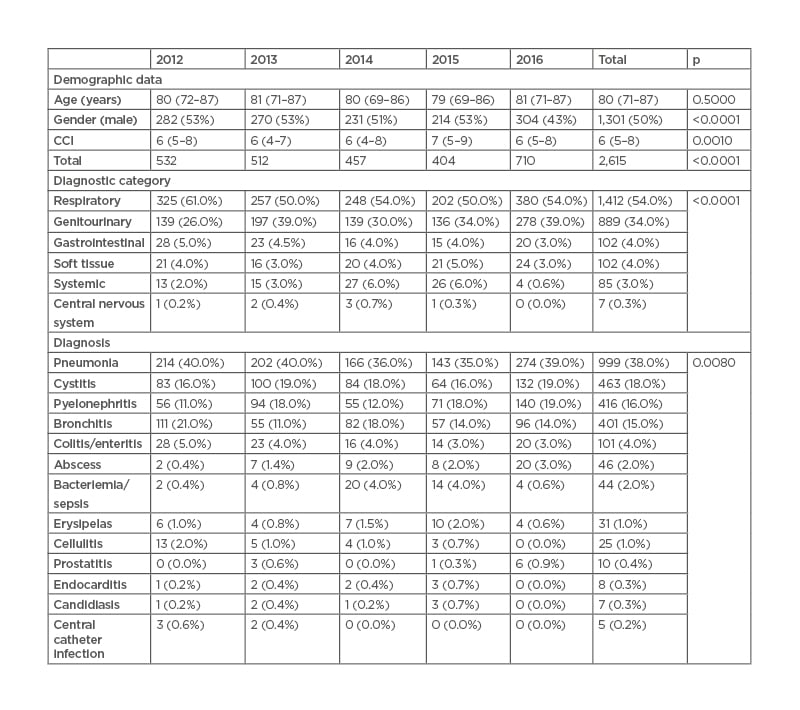
Table 1: Demographic data and diagnosis characterisation trends from 2012 to 2016.
CCI: Charlson Comorbidity Index.
There were 45 agents identified in total, including bacteria, virus, parasites, and fungus. The top 18, with an overall prevalence over 1%, were Escherichia coli (29.0%), Pseudomonas aeruginosa (9.0%), Klebsiella pneumoniae (7.0%), E. coli extended-spectrum β-lactamase (ESBL; 6.8%), methicillin-resistant Staphylococcus aureus (MRSA; 6.7%), Enterococcus spp. (5.0%), Proteus mirabilis (4.2%), pneumococcus (4.1%), methicillin-sensitive S. aureus (3.9%), Enterobacteriaceae spp. (3.6%), Candida albicans (2.3%), K. pneumoniae ESBL (2.1%), Clostridium difficile (1.7%), Candida spp. (1.4%), Morganella morganii (1.3%), Streptococcus spp. (1.3%), influenza virus (1.2%), and Acinetobacter baumannii (1.1%). Of these agents, a marginally significant trend was observed (p=0.057), with a reduction in E. coli, MRSA, Enterococcus spp., and A. baumannii, and an increase in P. aeruginosa, E. coli ESBL, Enterobacteriacea spp., and K. pneumoniae ESBL (Table 2).
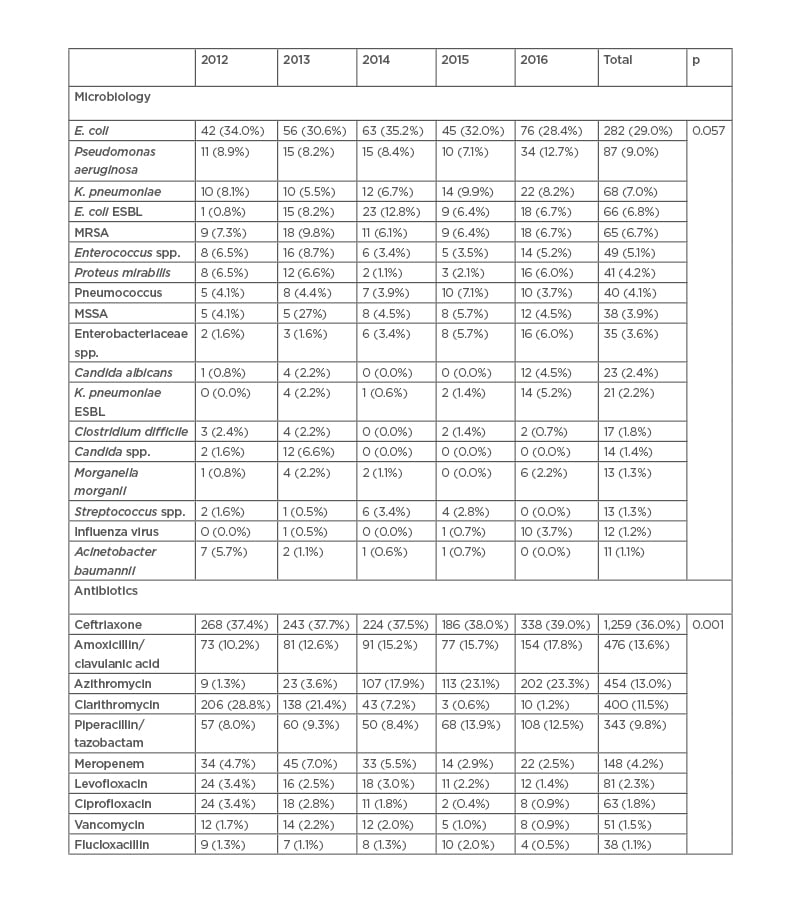
Table 2: Microbiologic isolation and antibiotic use trends from 2012 to 2016.
ESBL: extended-spectrum β-lactamase; E. coli: Escherichia coli; K.
pneumoniae: Klebsiella pneumoniae; MRSA: methicillin-resistant
Staphylococcus aureus; MSSA: methicillin-sensitive Staphylococcus aureus.
Over 30 different antibiotics were used, either alone or in combination as a first-line therapy for these infections. The 10 most frequent (overall prevalence of over 1%) were ceftriaxone (36.0%), amoxicillin/clavulanic acid (13.6%), azithromycin (13.0%), clarithromycin (11.5%), piperacillin/tazobactam (9.8%), meropenem (4.0%), levofloxacin (2.3%), ciprofloxacin (1.8%), vancomycin (1.5%), and flucloxacillin (1.0%). There was a significant trend (p=0.001) with increased use of azithromycin with a simultaneous decline in clarithromycin use. Moreover, there was also an overall rise in ceftriaxone and amoxicillin/clavulanic acid, together with piperacillin/tazobactam use, compared with a decreased use of meropenem, levofloxacin, ciprofloxacin, vancomycin, and flucloxacillin (Table 3).
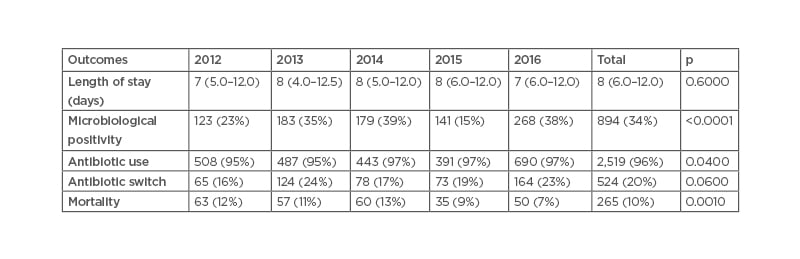
Table 3: Outcome trends from 2012 to 2016.
Considering the outcomes (Table 3), the length of stay was, overall, unchanged (median: 8 days [interquartile range: 6–12 days]; p=0.6). Though not statistically significant, there was a growth in antibiotic switch from 16% to 23% (p=0.06). Antibiotic usage also increased from 95% to 97% (p=0.04), along with microbiologic positivity (23% to 38%; p<0.0001). Contrasting, mortality declined from 12% to 7% (p=0.001).
DISCUSSION
In the authors’ short-term (5 year) assessment of IDs trends, they found that its incidence as the sole admission motive is diminishing. However, the authors have not taken into account IDs as a second diagnosis, decompensating chronic pathologies such as heart failure or chronic obstructive pulmonary disease, which could lead to underestimation despite a slight increase in the CCI, with observed a sustained population age of 80 years. Respiratory and genitourinary infections are the most prevalent, and follow an opposite tendency, with one decreasing and the other increasing. As genitourinary infections were more prevalent in elderly females with more comorbidities and with decreased functional impairment rate, that increased during the 5 years.
The most frequent agents remain bacteria, with an emphasis on Enterobacteriaceae; however, attention should be paid to the influenza virus and Candida, as well. It was interesting to observe the raise in ESBL Enterobacteriaceae, with concomitant decline in MRSA and A. baumannii. This data is in line with international data regarding these agents.11
As far as antibiotic use goes, there was a significant increase, which could lead to healthcare-associated infections;12 however, the core issue remains: the use of narrow-spectrum antibiotics as first-line empiric drugs, despite the rise in frequency of in-hospital ESBL agents, which can be related to the authors’ infection control programme efforts. The shift from clarithromycin to azithromycin was the result of changes of the hospital protocol for respiratory infections, from the infection control programme. This in-hospital programme elaborates a series of acting protocols regarding suggested antibiotics for common infections, together with annual reports regarding microbiology resistances. They also implement infection control measures such as hand-washing inspections, aseptic measures, and control over broad-spectrum antibiotics.
One of the most striking outcome results was the increase in microbiologic positivity from 23% to 38%, justified by adequate collection of cultural samples and the continuous improvement of laboratory techniques, which helps to proceed with antibiotic switch or maintenance more accurately. Also of note is the decrease of in-hospital mortality, without significative shift in the hospital length of stay, which could be related to both a higher and accurate use in antibiotics, the increase in microbiologic positivity, and infection control policies. The author’s decrease in mortality contrasts with data from South Korea, which documented an increase in mortality in the elderly population.13
The authors’ main bias is the short duration of the study, as 5 years can be insufficient for some trends to establish as well as its retrospective nature. Also, it would have been of interest to perform some economic analysis on the burden of these tendencies as to help in health policies changes. However, the authors do believe this analysis is important, even if just on a local point of view, to establish prevalences and resistances.