Abstract
Multisystem inflammatory syndrome (MIS-C) is a challenging disease associated with COVID-19. Clinical manifestation of MIS-C may mimic many endemic illnesses of tropical and subtropical countries, making early diagnosis more difficult. The authors present the case of an 8-year-old who presented with non-specific febrile illness which was managed as extensively drug-resistant typhoid with meropenem. The patient developed abdominal pain and hypotension during the hospital stay. Surgical causes were ruled out and managed with fluid protocol of dengue shock syndrome on the basis of falling platelets and fluid leak on ultrasound. But refractory condition and new-onset cardiac dysfunction prompted alternate diagnosis. Diagnostic criteria of MIS-C were fulfilled and the patient was managed with a single dose of intravenous Ig, pulse therapy of methylprednisolone, and temporary pacemaker placement. MIS-C should be kept in the differentials of diseases with multisystem involvement in the wake of the COVID-19 pandemic, as its clinical spectrum closely mimics other endemic illnesses of tropical and subtropical regions.
Key Points
1. In the wake of the COVID-19 pandemic, multisystem inflammatory syndrome in children should be kept in the differentials of all tropical fevers by paediatricians.2. Meticulous clinical examination and relevant laboratory investigations will not only aid in early diagnosis, but also help in prompt management.
3. Multisystem inflammatory syndrome is a challenging medical condition, but appropriate management can cause positive impact on its outcome.
INTRODUCTION
Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 has become increasingly recognised worldwide. Early identification is crucial owing to its severe multiorgan involvement and lethal outcomes. It has been reported 2–4 weeks post-COVID-19, and attributed to immune response to severe acute respiratory syndrome coronavirus 2.1 Clinical presentations of this disease can cause variable organ involvement as the pandemic emerges. It may overlap with many endemic illnesses in tropical regions, and it can be difficult to differentiate COVID-19 with dengue due to similar laboratory parameters.2 Thus, the impact of both dengue and COVID-19 can lead to devastating consequences in tropical and subtropical areas worldwide.3 The authors report the case of an 8-year-old patient who had an unusual course of disease, managed from enteric fever turned dengue shock syndrome, and eventually fulfilled the criteria of MIS-C. To the best of the authors’ knowledge, there are no cases reported from Pakistan regarding MIS-C mimicking other endemic illnesses of tropical countries.
CASE PRESENTATION
Patient Information and Clinical Findings
A thriving 8-year-old male presented in the outpatient department of the Khan Research Laboratories (KRL) Hospital, Islamabad, Pakistan, with the complaint of fever for 4 days. The patient was already taking oral antibiotics prescribed by a general practitioner, but had not improved. He was brought into hospital with a high-grade fever. He did not have a cough, abdominal pain, vomiting, headache, or skin rash. Past history was also insignificant. Examination was unremarkable except some dehydration.
Diagnostic Assessment
Laboratory workup was sent, as shown in Table 1, and the patient was managed with intravenous ceftriaxone; however, his fever progressively increased to 103 °F. Keeping in mind the multidrug-resistant enteric fever endemic in Pakistan, the patient was switched to meropenem on Day 2 of admission, awaiting blood culture report.
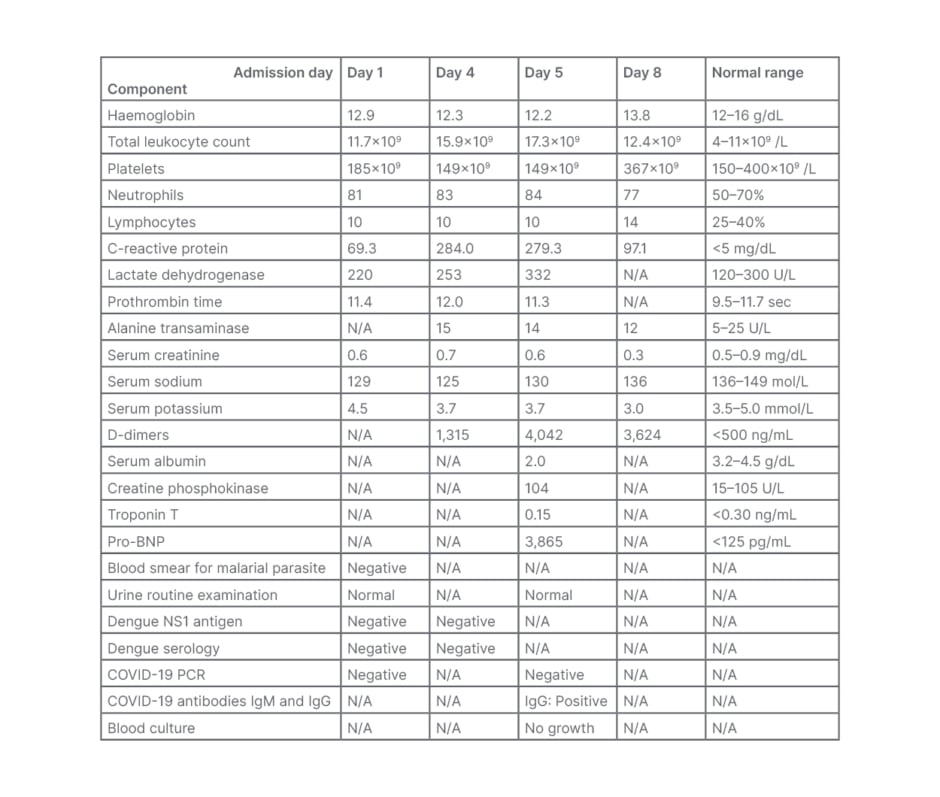
Table 1: Significant laboratory results during stay in hospital.
BNP: B-type natriuretic peptide; N/A: not applicable; NS1: non-stuctural protein 1.
On Day 4 of admission, the patient developed abdominal pain which continued to worsen. He had tachypnea (respiratory rate 44 /min), tachycardia (110 /min), oxygen saturation of 96% in air, and blood pressure of 95/56 mmHg which was below the 50th centile for the patient’s age, gender, and height. The patient had abdominal tenderness more in the epigastric region with no visceromegaly. Chest and neurological examination was unremarkable. Blood tests were repeated (Table 1); erect X-ray and ultrasound abdomen was also done to rule out enteric perforation. Erect X-ray negated abdominal perforation. Ultrasound abdomen showed evidence of dengue leak syndrome in the form of mild left side pleural effusion, gall bladder thickness of 4 mm, and mild free fluid in the pelvis. The blood complete picture showed thrombocytopenia, with falling trend of haematocrit (from 37.0% to 29.6%), which also supported dengue. Clinical scenario of tachycardia, cold peripheries, and pulse pressure of 20 mmHg, along with signs of plasma leak, prompted immediate management of dengue shock syndrome. The patient required two crystalloid and one colloid bolus along with red cell concentrates to improve urine output.
After 18 hours of fluid management, the patient again became hypotensive with narrow pulse pressure and increased work of breathing. The patient was reassessed for complications of severe dengue, and relevant blood work was sent (Table 1, Day 5). The ECG showed low voltage QRS complexes. Echocardiography revealed global hypokinesia and left ventricular dysfunction with ejection fraction of 30%, but no coronary abnormalities (Z-score <2 for the patient’s age). Norepinephrine infusion at 0.1 mcg/kg/min was started to improve blood pressure while awaiting blood results. Various causes of acute myocarditis were explored as non-structural protein 1 antigen and dengue serology came back negative. The patient’s clinical presentation of hypotensive shock, cardiac dysfunction, and acute gastrointestinal symptoms in the setting of the COVID-19 pandemic strongly indicated the possibility of MIS-C. This was supported by negative blood cultures, elevated markers of inflammation (C-reactive protein, lactate dehydrogenase, D-Dimers, neutrophilia, and hypoalbuminaemia), and evidence of severe acute respiratory syndrome coronavirus 2 in the form of positive IgG levels.
Therapeutic Intervention
The rapidly progressive nature of MIS-C in this patient in the form of worsening respiratory distress and hypotension was managed with intravenous Ig (IVIg) at the dose of 1 g/kg. IV dexamethasone was also given to hasten improvement. Meanwhile, CT scan was advised and serial blood tests were done to see multiorgan complications (Table 1, Day 5). The CT showed moderate bilateral pleural effusion and non-segmental areas of collapse in basal segments. There was no significant improvement 12 hours post-IVIg administration, and the patient’s clinical status warranted elective intubation. Dexamethasone was shifted to pulse therapy of methylprednisolone (30.0 mg/kg/dose) and anticoagulation therapy (enoxaparin 0.5 mg/kg/day subcutaneously). The patient was also reconsidered for a second dose of IVIg or immunomodulation therapy. Meanwhile, the patient’s heart rate started to fluctuate between 60–80 beats per min, and serial echocardiography showed similar results. The paediatric cardiology team advised urgent placement of a temporary pacemaker due to sinus bradycardia with haemodynamic impairment. After temporary pacemaker placement and inotropic support, successful extubation was achieved after 24 hours, and repeat echocardiography showed improving ejection fraction. Treatment was revised to oral steroids and aspirin, and the patient was weaned off from pacemaker 4 days after its placement. Patient length of stay was prolonged due to post-extubation lung collapse, but this was managed with antibiotics and physiotherapy.
Outcome
Echocardiography at the time of discharge showed a structurally and functionally normal heart. The patient was discharged on tapering dose of steroids and aspirin on Day 18 of admission. Follow-up was advised to keep an eye on their cardiac status.
DISCUSSION
COVID-19 is a public health crisis worldwide, but as it shares a similar clinical spectrum with other viral illnesses, it has become a major threat for dengue-endemic countries in particular.4 Pakistan is also facing the major disease burden of drug‐resistant typhoid cases, and the estimated attack rate of typhoid is considered to be 15.5 out of 10,000 of the population. Due to non-specific presentation of typhoid, it can easily be confused with other illnesses like malaria, dengue, and COVID‐19. It has been difficult to diagnose many illnesses in resource-limited settings without performing relevant diagnostic tests and, in the wake of COVID‐19 pandemic, healthcare professionals are facing difficulties in differentiating these illnesses due to common manifestations.5 This case highlights the diagnostic dilemma of a paediatric patient who presented with non-specific febrile illness.
Around 129 countries are at risk of dengue infection, as the disease is endemic in more than 100 countries. Asia contains 70% of the real disease burden.2 Pakistan has reported around 99,264 confirmed cases of dengue virus infection from January 2014–May 2020 from all provinces, with major outbreaks observed between July and December.6 Non-specific symptoms of dengue may include fever, respiratory tract infection, and rash; however, maculopapular rash, body aches, and high-grade fever are more typical symptoms. The spectrum of illness may vary, from mild disease such as dengue fever to dengue haemorrhagic fever and dengue shock syndrome, which can lead to adverse complications.7 The authors’ patient was managed as dengue shock syndrome due to hypotension and ultrasonographic findings of fluid leak, delaying the final diagnosis due to high disease burden of dengue epidemic in the region. However, cardiac and gastrointestinal involvement, along with shock in the setting of fever, supported with laboratory evidence of positive COVID-19 IgG antibodies and clear blood cultures, fulfilled the case definition of MIS-C by the World Health Organization (WHO).8
A case reported from Indonesia supported the similar case presentation of MIS-C and dengue, but with positive dengue infection ultimately resulting in mortality of the patient.9 However, the authors’ patient survived myocardial decompensation of MIS-C, thanks to the evolving management of MIS-C. Similarly, a case has been reported from India of a 9-year-old male who was managed as MIS-C, presented initially with dengue-like illness, and was discharged with a better outcome.10 Cases have also been reported about co-infection of COVID-19 with other febrile illnesses. A study carried out in Bangladesh showed 40% of the study population had typhoid fever with COVID-19. Co-infections along with comorbidities are a great matter of concern during this pandemic.11 Due to the evolving nature of COVID-19, a study conducted about the clinical characteristics of MIS-C showed that about 54% patients required treatment with IVIg, 51% with steroids, 21% with remdesivir, 36% with tocilizumab, and 51% required vasopressors. Meticulous examination and critical care is required to achieve good outcomes in patients with MIS-C.12 However, ongoing studies on MIS-C will help clinicians in understanding its varied clinical manifestations.







