Abstract
Filariasis is a common public health problem in Southeast Asia. The two species of worms most commonly associated with this disease are Wuchereria bancrofti and Brugia malayi.
Cases of microfilaraemia have also been reported from atypical sites in the past. None of the previously reported cases of microfilaria in the thyroid gland have described occult filariasis against a background of lymphocytic thyroiditis. The authors present a case of incidental microfilaria in a case of lymphocytic thyroiditis, diagnosed on fine needle aspiration cytology of thyroid swelling in a female, a coexistence of dual pathology. There has been no case in literature where filariasis was reported against a background of lymphocytic thyroiditis. Peripheral blood examination also did not show any evidence of filariasis.
Key Points
1. Filariasis is a common public health problem in Southeast Asia. There are as many as 60 million people infected in the region, and approximately 31 million people have the clinical manifestation of this disease.
2. This article presents a case of microfilaria in a case of lymphocytic thyroiditis diagnosed on fine needle aspiration cytology (FNAC) of thyroid swelling in a female, a coexistence of dual pathology.
3. This case report reiterates the importance of FNAC in the diagnosis of occult filariasis in an uncommon site like the thyroid gland. Thus, it is worth noting that with a simple procedure of FNAC, a coexistence of dual pathology was identified in an asymptomatic case. It also emphasises the significance of careful screening of smears in an endemic area.
INTRODUCTION
Filariasis is an infectious disease caused by any one of various parasitic roundworms. Wuchereria bancrofti and Brugia malayi are the two most frequent causative organisms of filariasis.1 Filariasis is a public health problem in Southeast Asia, with as many as 60 million people infected, and 31 million people exhibiting clinical manifestation of this disease.1 The disease is endemic in all parts of India, particularly in Bihar, Jharkhand, Uttar Pradesh, Andhra Pradesh, Orissa, and Tamil Nadu.1, 2
There have been few cases of microfilaraemia reported in uncommon sites, such as in breast lumps, pleural/pericardial fluid, lymph nodes, and bone marrow. The authors present a case of microfilaria in a case of lymphocytic thyroiditis diagnosed on fine needle aspiration cytology (FNAC) of thyroid swelling in a female, a coexistence of dual pathology.
CASE REPORT
A 40-year-old female, resident of Bihar, first presented to the outpatient department with complaints of painful anterior neck swelling for 2 months. The patient was of average build with stable vitals and no lymphadenopathy.
Thyroid examination revealed a Grade 3 asymmetrical goiter (right lobe>left lobe) with firm consistency and smooth surface. However, it was non-tender on palpation. The patient was further advised for radiological examination and a thyroid profile test.
A neck ultrasound revealed enlargement of both lobes of the thyroid, with a few Thyroid Imaging Reporting and Data Systems (TIRADS) 3 nodules of size 5×6 mm in the left lobe, suggestive of thyroiditis. The thyroid profile test showed elevated thyroid stimulating hormone (Table 1).
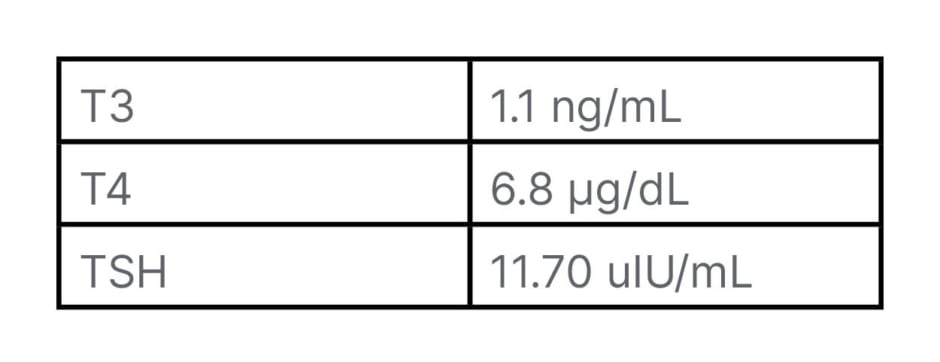
Table 1: Thyroid profile of patient.
T3: triiodothyronine; T4: thyroxine; TSH: thyroid-stimulating hormone.
FNAC was done and yielded a blood mixed aspirate. The Giemsa-stained smears were cellular, and showed thyroid follicular cells with lymphocyte impingement along with focal Hürthle cell change (Figure 1A, 1B). Smears also showed the presence of sheathed, coiled, and slightly curved microfilaria (Figure 1C) against a background of scant colloid. A final diagnosis of filariasis in a case of lymphocytic thyroiditis was made.
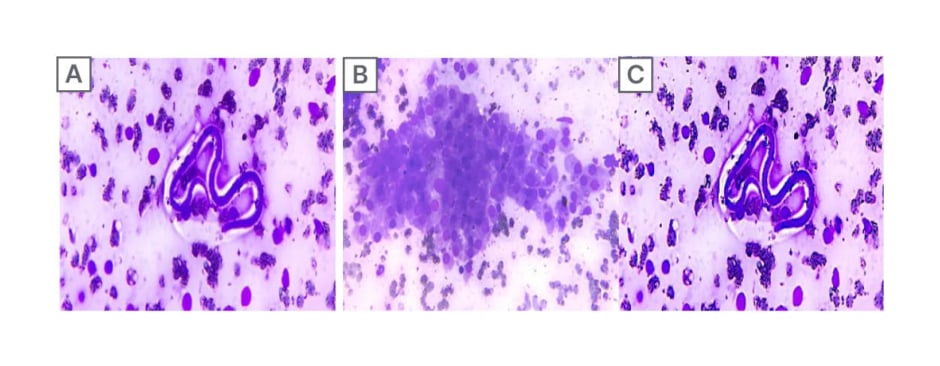
Figure 1: Cytomorphological findings.
A) Thyroid follicular cells with microfilaria marked with red arrow (40x magnification; Giemsa stain).
B) Thyroid follicular cells with lymphocytic impingement with Hürthle cell change (200x; Giemsa stain).
C) The sheathed curved microfilaria against a background of scattered follicular cells (200x; Giemsa stain).
The patient was advised serological testing for anti-thyroid peroxidase (anti-TPO) antibodies and peripheral blood film examination. Post-FNAC, serological investigations revealed an elevated level of anti-TPO antibodies, which favoured the coexistence of Hashimoto thyroiditis with occult filariasis. However, the peripheral blood smears were unremarkable, but showed mild eosinophilia.
The patient was treated with diethyl carbamazepine for 6 months, which led to a mild reduction in size of the swelling.
DISCUSSION
Filariasis is a major public health problem in Southeast Asian countries. It is endemic in a few regions of India, particularly in Bihar, Jharkhand, Uttar Pradesh, Andhra Pradesh, Tamil Nadu, Gujarat, Orissa, and Kerala.1
Most infected individuals in filarial endemic areas are asymptomatic. Adult worms are known to reside in the lymphatic vessels of the definitive host, from where microfilaria are released to circulate in the peripheral blood. The disease is transmitted by the larval form through mosquito bite. Early symptoms include fever with chills, headache, and skin lesions.3,4
The presence of microfilaria against a background of lymphocytic thyroiditis is a rare finding, with very limited data available. None of the cases which have reported filariasis in the thyroid observed a background of lymphocytic thyroiditis.
The present case is an uncommon presentation, since the patient presented with diffuse anterior neck swelling, which showed presence of microfilaria with evidence of lymphocytic thyroiditis with elevated anti-TPO antibodies, leading to a diagnosis of occult filariasis in a case of Hashimoto thyroiditis. However, in the present case, the patient was an asymptomatic carrier, with larvae present in the microvasculature of the thyroid gland. Few studies have proposed a possible mechanism of rupture of vessels, leading to haemorrhage and release of microfilaria into the thyroid. However, the presence of microfilaria against a background of lymphocytic thyroiditis is a rare finding in itself.1,2,5 This case report reiterates the importance of FNAC in the diagnosis of an occult filariasis in an uncommon site like the thyroid gland. Thus, it is worth noting that with a simple procedure of FNAC, a coexistence of dual pathology was identified in an asymptomatic case. It also emphasises the importance of careful screening of smears, particularly in endemic areas.







